Gut Health and Hormones: The Hidden Connection
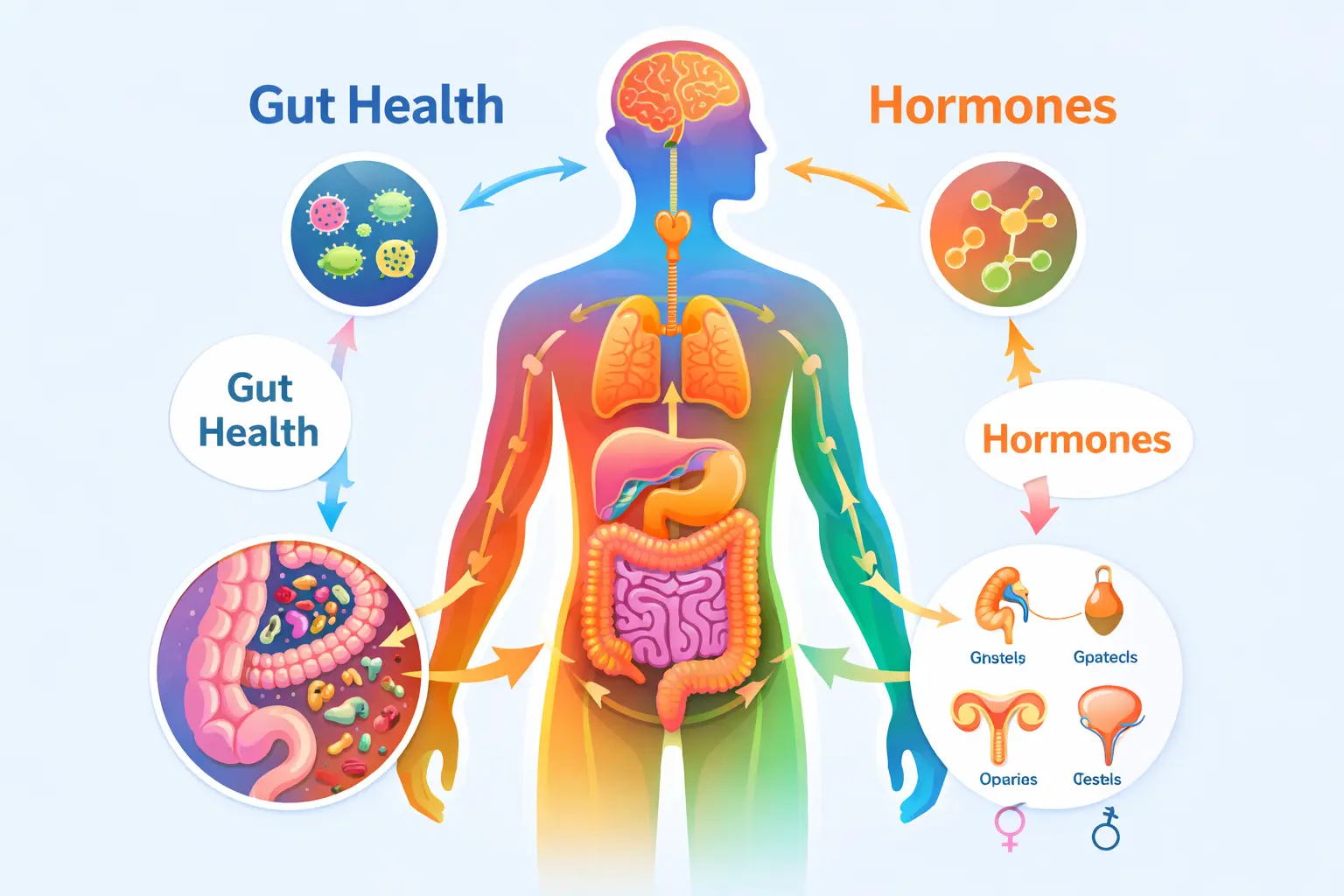
From my experience working with clients, one thing I’ve noticed is that gut health and hormones are more connected than most people realise. Many come in for digestive issues, unexplained fatigue, or mood changes, thinking these are separate problems. But the reality is, a healthy gut isn’t just about digestion — it plays a key role in regulating hormones, metabolism, stress response, energy levels, and even mental well-being.
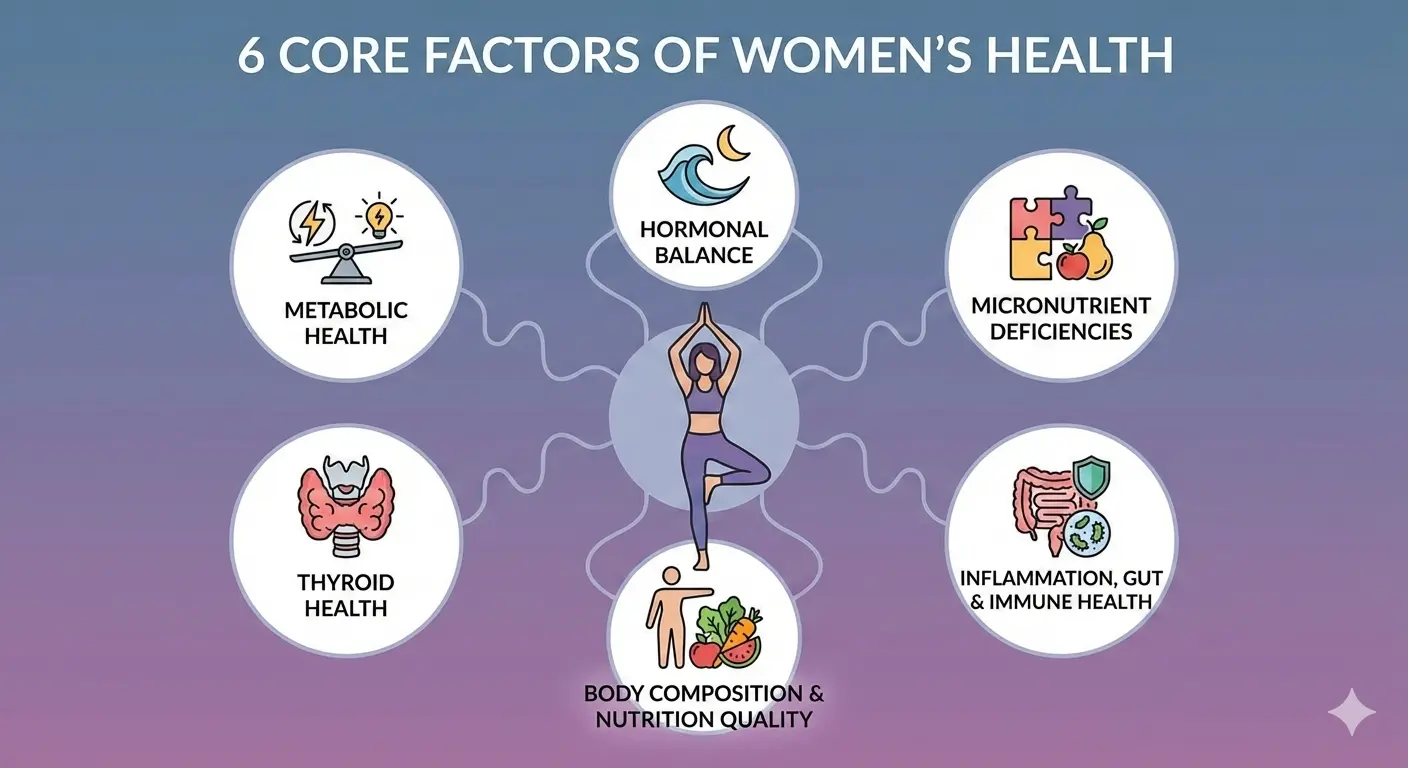
A disrupted gut microbiome can quietly affect hormone balance, creating a ripple effect across the body. Understanding this hidden connection is the first step toward addressing root causes rather than just managing symptoms. Gut health is also recognised as one of the core factors influencing women’s health .
Why Gut Health Matters More for Women
The gut is often called the “second brain” not just because it contains millions of nerve cells, but because it communicates constantly with other body systems through hormones, neurotransmitters, and immune signals.
In women, hormonal changes across the menstrual cycle, pregnancy, postpartum, and menopause add layers of complexity to this gut–brain–hormone connection. When the gut microbiome is imbalanced (a state known as dysbiosis), symptoms may show up as irregular cycles, PMS, weight gain, fatigue, and mood swings — even when diet and sleep appear adequate.

What Is Gut Health? Beyond Digestion
Gut health refers to the state of the trillions of microorganisms — bacteria, viruses, and fungi — living in the digestive tract, collectively known as the gut microbiome, along with the integrity of the gut lining itself.
Beyond digestion, the gut produces neurotransmitters such as serotonin and GABA, influences immune responses, and communicates bidirectionally with the endocrine system. This means gut imbalance can disrupt hormonal rhythms, while hormonal imbalance can also impair gut function.
The Gut–Hormone Connection in Women
Estrogen Metabolism and the Estrobolome
The gut harbours a unique group of microbes known as the estrobolome — bacteria capable of metabolising and recycling estrogen. These microbes determine whether estrogen is eliminated or reabsorbed into circulation.
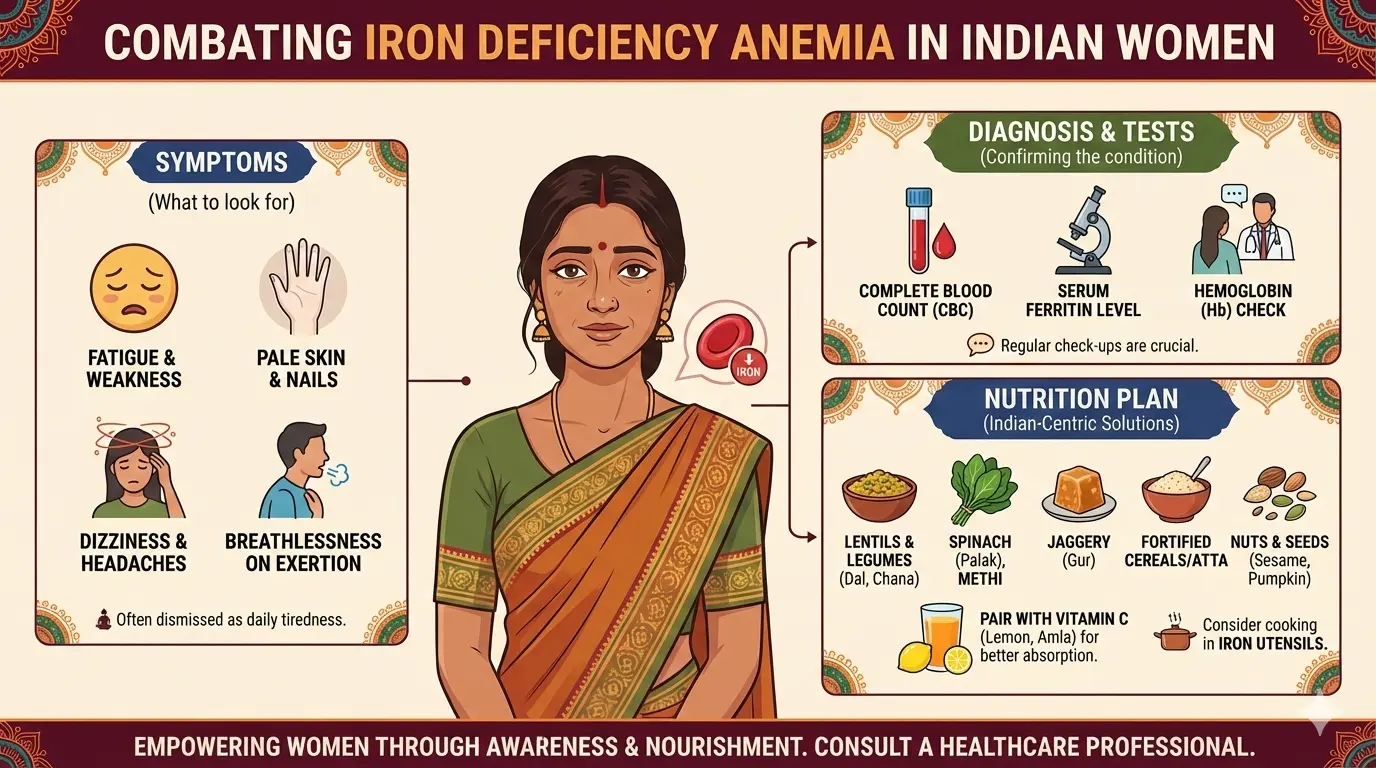
When gut balance is disrupted, excess estrogen may be reabsorbed, contributing to symptoms such as heavy periods, PMS, fibroids, endometriosis, and PCOS-related hormonal imbalance .
Gut Health and Insulin Sensitivity
The gut microbiota influences metabolic hormones such as insulin, GLP-1, leptin, and peptide YY. Short-chain fatty acids (SCFAs) produced by gut bacteria help improve insulin sensitivity and reduce inflammation.
An imbalanced microbiome may contribute to insulin resistance , a key driver of metabolic dysfunction and type 2 diabetes.
Gut–Thyroid Axis
Approximately 20% of the conversion of inactive T4 hormone into active T3 occurs in the gut. Dysbiosis and inflammation can impair this process, contributing to fatigue, weight gain, and metabolic slowdown even when thyroid tests appear normal.
You can explore this further in our detailed guide on thyroid hormone conversion and nutrition .
Hormones Influenced by Gut Health
| Hormone (Role) | How Gut Health Influences It | Common Symptoms When Imbalanced |
|---|---|---|
| Cortisol (Stress hormone) | Gut inflammation and increased permeability activate the stress response | Abdominal fat gain, anxiety, poor sleep, sugar cravings |
| Progesterone (Cycle-supporting hormone) | Dysbiosis and inflammation worsen estrogen dominance | PMS, irregular cycles, mood swings, poor sleep |
| Leptin (Satiety hormone) | Poor gut health contributes to leptin resistance | Constant hunger, overeating, weight-loss resistance |
| Ghrelin (Hunger hormone) | Gut imbalance and irregular meals disrupt ghrelin regulation | Frequent hunger, cravings, energy crashes |
| Serotonin (Mood hormone) | Majority of serotonin is produced in the gut | Low mood, anxiety, constipation, disturbed sleep |
| Melatonin (Sleep hormone) | Gut microbes influence circadian rhythm and melatonin production | Insomnia, poor sleep quality, daytime fatigue |
| IGF-1 (Growth & repair hormone) | Chronic gut inflammation impairs nutrient absorption and tissue repair | Poor recovery, muscle loss, metabolic slowdown |
Table: Hormones Influenced by Gut Health
Inflammation, Gut Permeability & Women’s Health
When gut microbes are disrupted, the gut lining may become more permeable, allowing toxins to enter the bloodstream. This triggers chronic inflammation that interferes with hormone signalling, insulin sensitivity, and thyroid function.
Inflammation also stimulates cortisol release, creating a cycle where hormonal imbalance worsens gut health and vice versa.
Nutrition That Supports Gut Health in Women
- High-fibre foods: whole grains, fruits, vegetables, legumes
- Fermented foods: yogurt, kefir, idli, dosa, sauerkraut
- Prebiotics: garlic, onions, bananas, oats
- Anti-inflammatory foods: turmeric, ginger, fatty fish
Hydration, regular meal timing, and mindful eating further support digestion and hormone metabolism.

Nutrigenomics and Gut Health
Every woman’s gut responds differently to food due to genetics, stress exposure, and microbiome composition. Nutrigenomics explains why some women thrive on certain foods while others experience bloating or inflammation.
A nutrigenomics-based personalised nutrition approach helps align diet with genetic and microbial needs rather than relying on trial-and-error.
When to Seek Professional Support
If symptoms such as fatigue, bloating, mood swings, irregular cycles, or unexplained weight changes persist, a comprehensive evaluation is recommended.
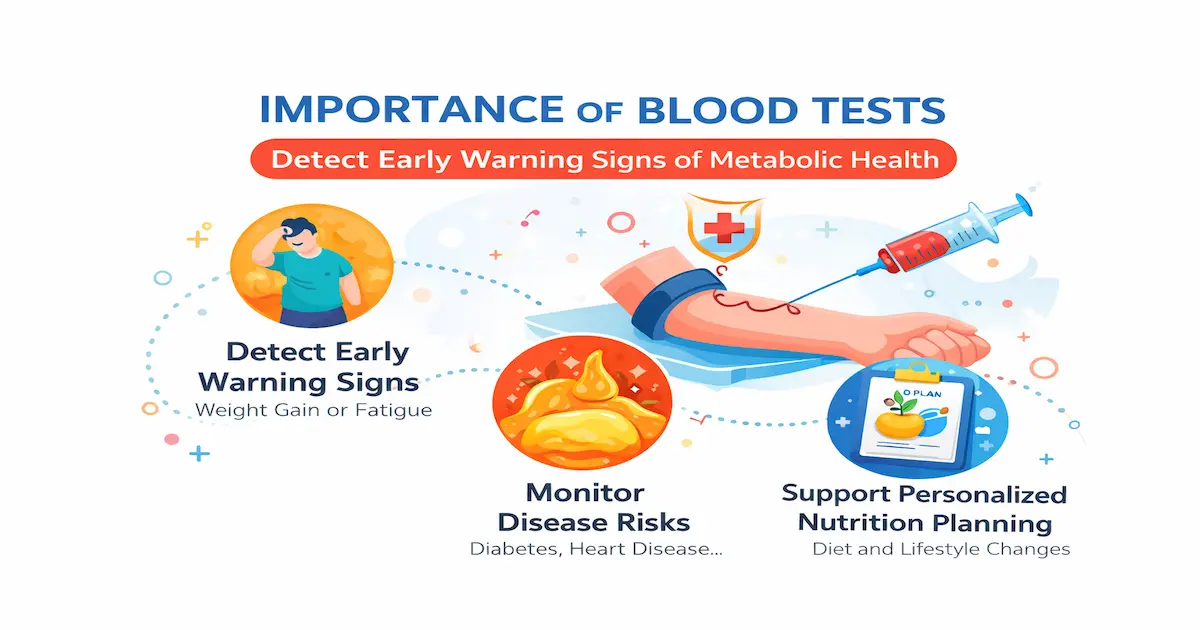
This often includes comprehensive blood testing , gut health assessment, and hormone profiling.
Final Takeaway
Gut health and hormones are deeply interconnected in women’s health. What happens in the digestive system affects metabolism, mood, immunity, and long-term well-being. Addressing gut health allows women to move beyond symptom management and toward sustainable balance.
References
-
Atoum M & Padma K. Gut microbiota–estrogen axis: Its influence on female health outcomes – A narrative review. Acta Biomed.
https://www.mattioli1885journals.com/index.php/actabiomedica/article/view/15980 -
Interaction between gut microbiota and sex hormones and their relation to sexual dimorphism in metabolic diseases.
Biology of Sex Differences.
https://link.springer.com/article/10.1186/s13293-023-00490-2 -
The impact of the gut microbiota on the reproductive and metabolic endocrine system.
PubMed.
The impact of the gut microbiota on the reproductive and metabolic endocrine system – PubMed -
Estrogen–gut microbiome axis: Physiological and clinical implications.
PubMed.
Estrogen–gut microbiome axis: Physiological and clinical implications – PubMed -
The relationship between thyroid and human-associated microbiota: A systematic review of reviews.
Reviews in Endocrine and Metabolic Disorders.
https://link.springer.com/article/10.1007/s11154-023-09839-9
Frequently Asked Questions (FAQs)
- Can gut issues contribute to PCOS or insulin resistance?
- Yes. Poor gut health can increase inflammation and impair insulin sensitivity. This can worsen blood sugar control and androgen excess, both of which are key features of PCOS. Supporting gut health may help improve metabolic and hormonal outcomes.
- Does gut health affect mood and mental health in women?
- Absolutely. The gut–brain axis links gut microbes with neurotransmitters like serotonin and dopamine. Poor gut health can worsen anxiety, low mood, brain fog, and stress resilience, especially during hormonally sensitive phases such as PMS or perimenopause.
- Are probiotics enough to fix gut-related hormonal issues?
- Probiotics can help, but they are not a standalone solution. Long-term gut and hormone balance requires adequate fibre, protein, micronutrients, blood sugar stability, stress management, and addressing root causes like inflammation or food intolerances.
- Can improving gut health help with weight management?
- Yes. A healthy gut supports better insulin sensitivity, reduced inflammation, improved appetite regulation, and efficient energy metabolism—factors that are closely linked to sustainable weight management in women.
- Is bloating always a gut issue, or can it be hormonal?
- It’s often both. Hormonal fluctuations can slow digestion and increase water retention, while poor gut motility or dysbiosis can worsen bloating—especially around the luteal phase or PMS.
- Can antibiotics or frequent medications affect hormones via the gut?
- Yes. Repeated antibiotic use can disrupt beneficial gut bacteria, including those involved in estrogen metabolism and insulin sensitivity. This can indirectly worsen hormonal imbalance.
Book a Free Consultation
If you are experiencing persistent gut, hormonal, or metabolic symptoms and want clarity on the root causes, our experts at Unlock.fit can help. Book a free consultation to understand how personalised nutrition, gut support, and lifestyle strategies can restore balance and long-term health.