High Cortisol Slowing Your Metabolism? 7 Science-Backed Fixes
High Cortisol Slowing Your Metabolism? 7 Science-Backed Fixes
Stress is no longer an occasional experience. For many women, it has become a constant background state—deadlines, caregiving, career pressure, irregular meals, poor sleep, and emotional load all quietly add up. While stress may feel like it exists only “in the mind,” the body experiences it as a powerful biological signal.
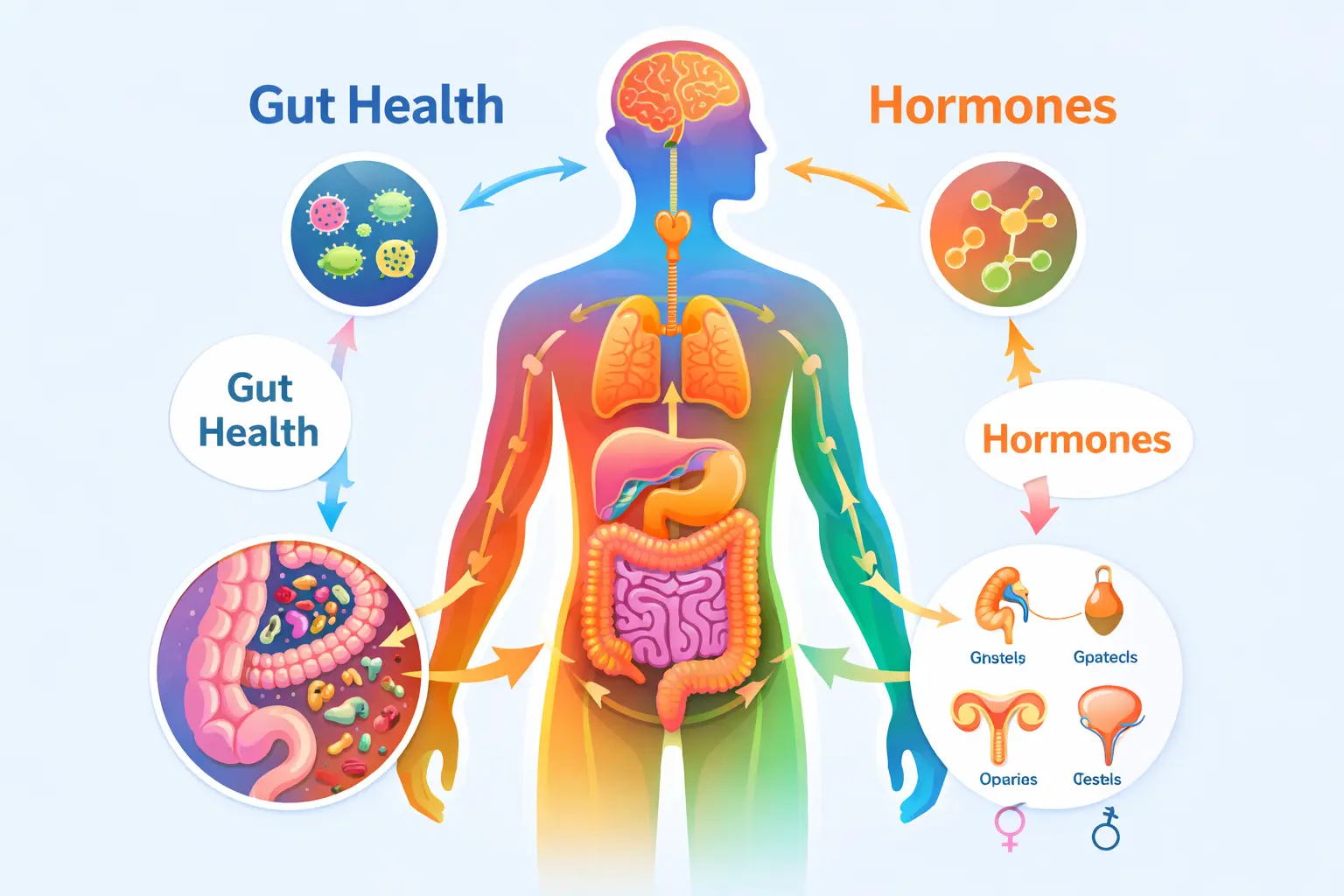
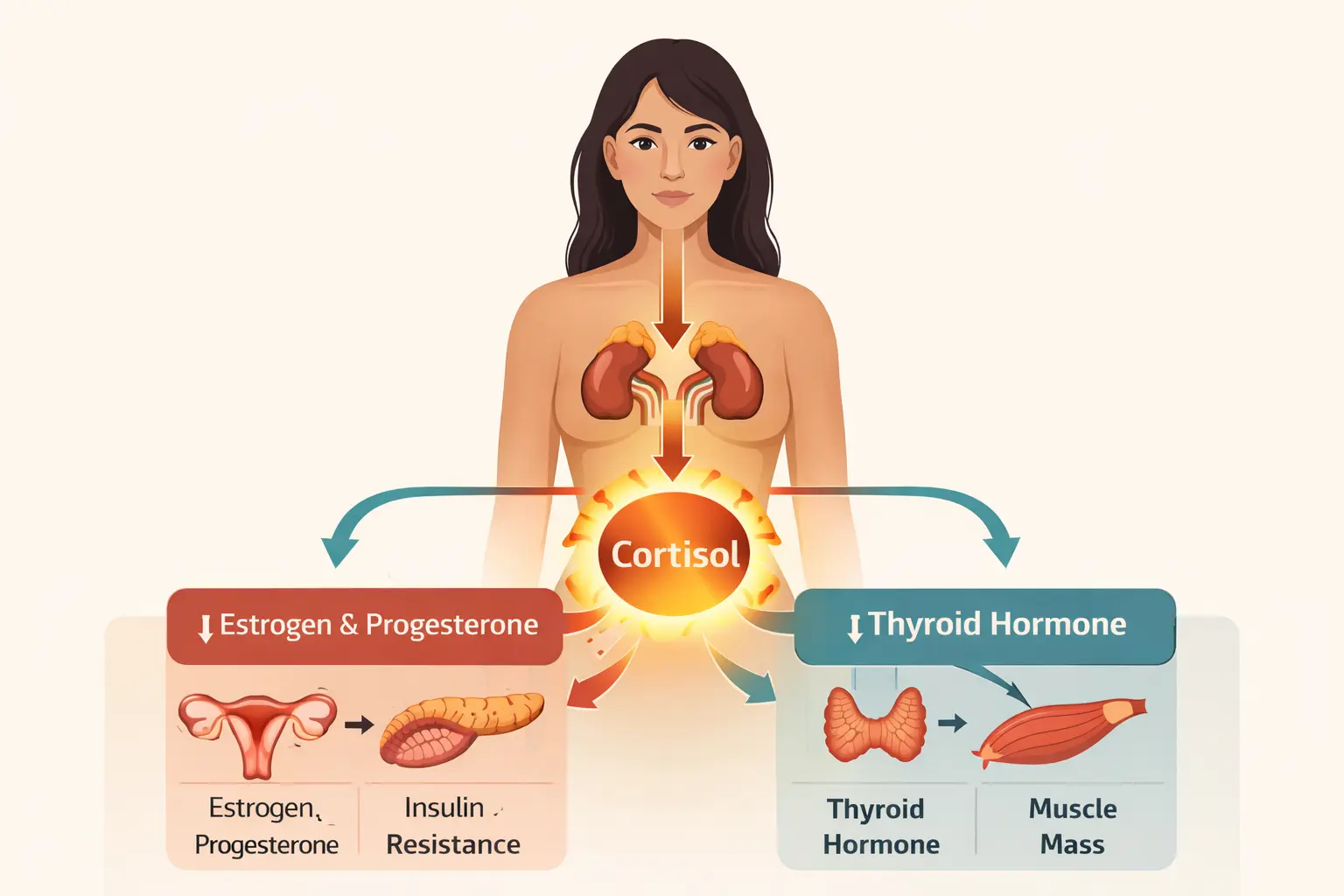
At the center of this response lies a complex triangle: stress hormones, metabolic hormones, and reproductive hormones. Cortisol, insulin, thyroid hormones, estrogen, and progesterone are in continuous communication with one another. When one shifts, the others adapt in response.
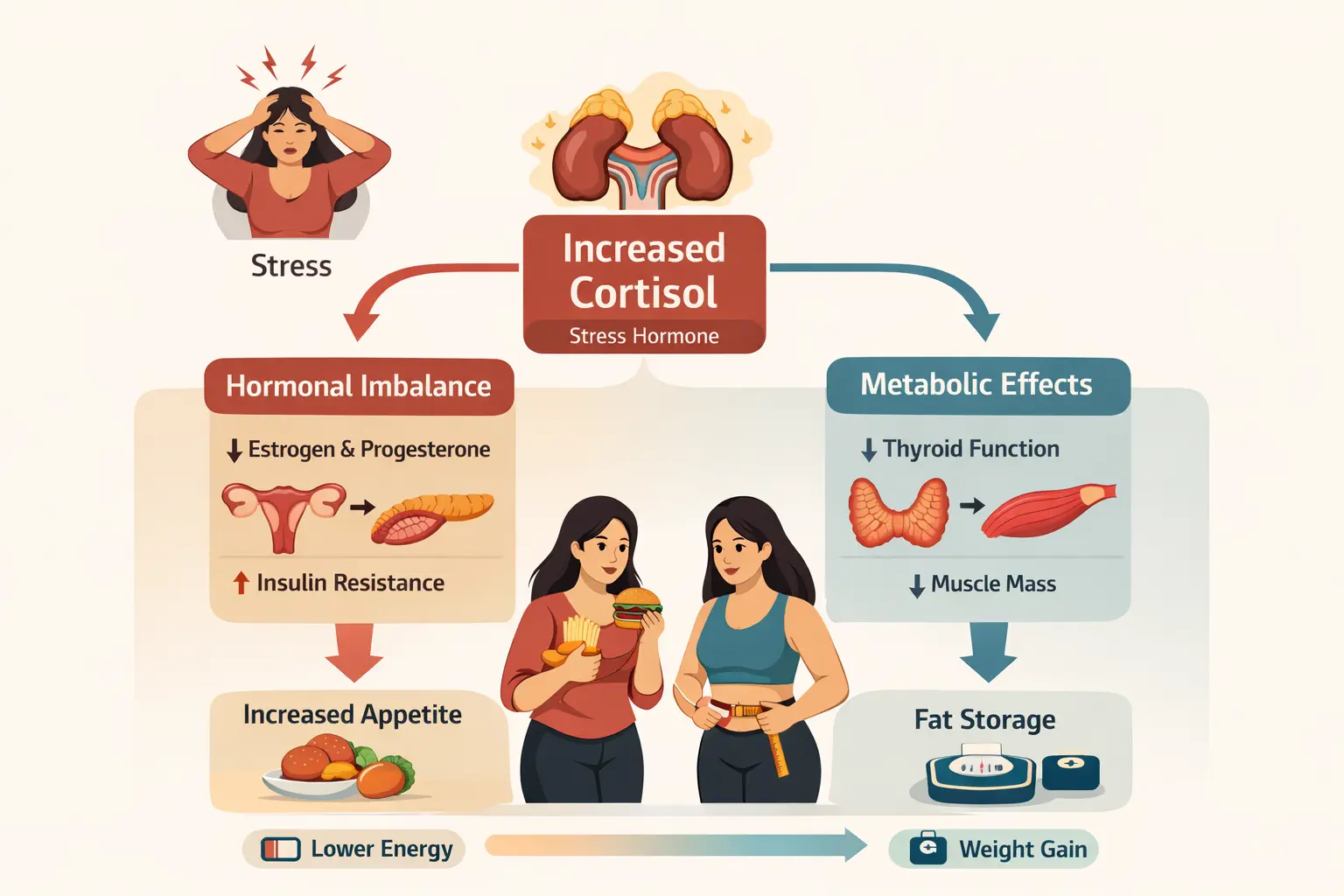
Cortisol, often called the stress hormone, is essential for survival. It helps the body wake up, stay alert, and respond to danger. But when stress becomes chronic, cortisol remains elevated for long periods. This constant hormonal signal can slowly reshape metabolism—affecting how the body stores fat, regulates appetite, maintains blood sugar, and supports reproductive health.
In women, this connection is especially delicate. Unlike men, women’s bodies are deeply influenced by cyclical hormonal changes, and stress can disrupt this rhythm in subtle but significant ways. Over time, the effects may appear as fatigue, weight gain, irregular cycles, cravings, and brain fog—symptoms that often feel disconnected but share a common root.
How Stress Affects Women’s Hormones
When the body perceives stress, the brain signals the adrenal glands to release cortisol. This is a protective mechanism designed to help us cope with challenges. In short bursts, cortisol is helpful—it increases focus, mobilizes energy, and supports quick responses.
But when stress is continuous, the body never fully returns to a calm state. Cortisol levels stay elevated, and this begins to interfere with other hormonal systems.
Chronic stress keeps cortisol levels elevated, which interferes with blood sugar regulation and insulin sensitivity .
The term “adrenal fatigue” is commonly used to describe the feeling of being constantly tired, wired, and unable to cope. While not a formal medical diagnosis, it reflects a real pattern of stress-response dysregulation. Over time, the body may struggle to maintain healthy cortisol rhythms, leading to energy crashes, mood fluctuations, and metabolic changes.
In women, chronic stress can disrupt communication between the brain and the reproductive system. The body prioritizes survival over reproduction, which can lead to:
- Irregular menstrual cycles
- Increased PMS symptoms
- Delayed ovulation
- Mood swings and irritability
Cortisol also influences insulin, the hormone responsible for blood sugar regulation. When cortisol remains high, the body may become more resistant to insulin, leading to frequent sugar cravings and energy crashes.
Another key effect is on fat storage. Elevated cortisol signals the body to store fat—especially around the abdomen. This evolutionary response ensured survival during prolonged stress, but in modern life it often translates into stubborn belly fat that feels resistant to diet and exercise.
Stress can also impair thyroid hormone function. Even when thyroid test results fall within the normal range, chronic stress may slow the conversion of thyroid hormones into their active forms, contributing to fatigue, cold intolerance, and metabolic slowdown.
Role of Sleep in Hormonal Health

Sleep is one of the most powerful regulators of hormonal balance, yet it is often the most neglected.
During sleep, the body repairs, restores, and resets hormonal rhythms. Cortisol follows a natural daily cycle—it rises in the morning to help us wake up and gradually declines throughout the day. Poor sleep disrupts this rhythm, keeping cortisol elevated when it should be falling.
Lack of sleep directly affects insulin sensitivity. When sleep is compromised, the body becomes less efficient at managing blood sugar. This can lead to higher glucose levels, stronger cravings, and increased fat storage over time.
Sleep also plays a major role in appetite regulation through two key hormones:
- Ghrelin, which signals hunger
- Leptin, which signals fullness
When sleep is inadequate, ghrelin levels increase while leptin levels decrease. This makes a person feel hungrier while reducing satiety, often leading to overeating—especially high-sugar and high-carbohydrate foods.
Chronic poor sleep can also worsen thyroid function, contributing to fatigue, low mood, and metabolic slowing. Many women experience a loop where stress disrupts sleep, poor sleep worsens hormonal imbalance, and hormonal imbalance increases stress.
Signs Your Metabolism Is Under Stress
The body rarely sends one clear signal. Instead, it communicates through patterns and subtle changes. Common signs include:
- Persistent fatigue that does not improve with rest
- Strong cravings for sugar, caffeine, or carbohydrates
- Weight gain concentrated around the abdomen
- Difficulty losing weight despite diet and exercise
- Irregular or painful menstrual cycles
- Brain fog and reduced concentration
- Mood changes, irritability, or low motivation
These symptoms are often treated individually, but in many cases they are connected through the body’s stress response.
These stress-related imbalances often show up in blood markers long before visible symptoms appear.
When cortisol remains elevated, the body enters a protective mode. Energy is conserved, metabolism slows, and fat storage increases. This is not a failure of discipline—it is a biological adaptation.
Nutrition Strategies to Support Stress Hormones
Food has a direct impact on hormones. Balanced nutrition helps stabilize blood sugar, support energy, and reduce stress signals within the body.
Avoiding extreme dietary patterns is crucial. Skipping meals or eating too little during the day can increase cortisol and worsen evening cravings.
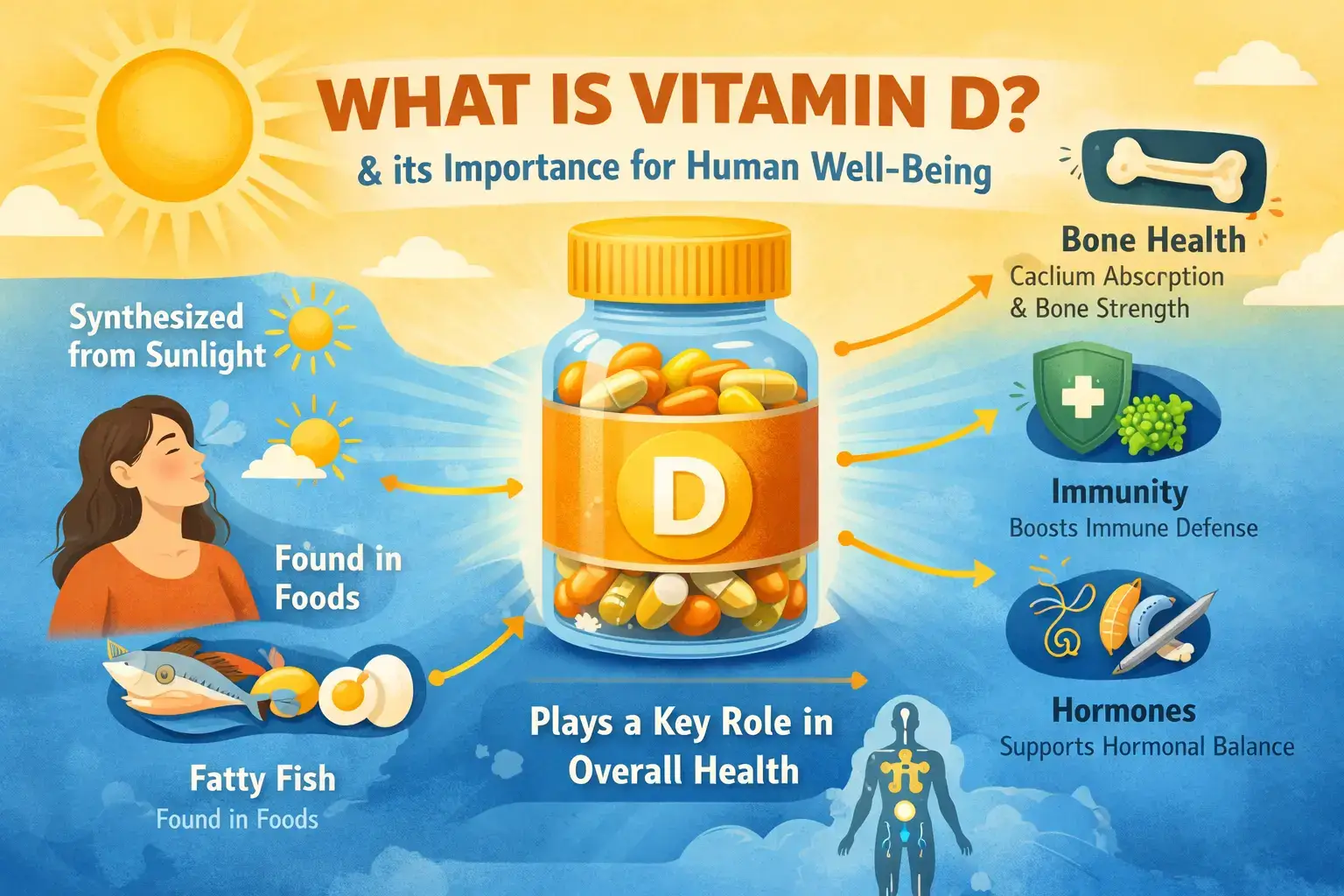
Balanced meals with protein, healthy fats, and complex carbohydrates help regulate blood sugar and prevent energy crashes. Omega-3 fatty acids (walnuts, flaxseeds, fatty fish) support brain health and reduce inflammation. Magnesium-rich foods (leafy greens, nuts, seeds, legumes) support the nervous system and sleep quality.
Habits that can worsen stress response include:
- Excess caffeine, which can increase cortisol and anxiety
- High sugar intake, leading to spikes and crashes
- Heavy late-night meals that disrupt sleep
Small, consistent changes are more effective than drastic diets.
DNA and Blood Insights for Stress & Metabolism
Women respond to stress differently, partly due to genetics. DNA insights may reveal tendencies such as:
- Higher stress sensitivity
- Slower caffeine metabolism
- Increased insulin resistance risk
- Differences in nutrient utilization
Blood tests add further clarity by assessing vitamin D, B12, iron, thyroid markers, and HbA1c.
Together, DNA and blood data provide a more complete picture of how stress affects the body and allow for personalized support.
Individual differences in stress response highlight the need for a personalised nutrition approach rather than generic advice.The Cortisol–Insulin Connection
Chronic stress raises cortisol, which increases blood glucose. Insulin then works harder to lower it. Over time, cells become less responsive, leading to insulin resistance.
This often appears as:
- Evening sugar cravings
- Energy crashes after meals
- Difficulty losing weight
- Increased abdominal fat
Cortisol signals “store energy,” while insulin stores glucose as fat. Together, they shift the body toward storage rather than burning.
Stress and the Female Body: A Protective Design
Women’s bodies are biologically sensitive to stress—a survival mechanism. During stress, the body may delay ovulation, alter cycles, increase PMS symptoms, and lower energy availability.
The body is not malfunctioning; it is responding intelligently to perceived pressure. But modern stress is constant, leaving little time for recovery.
Emotional Stress and Metabolism
Emotional stress has a powerful biological impact. Unprocessed mental load keeps the nervous system activated, affecting digestion, appetite, and nutrient absorption.
Chronic emotional stress can:
- Slow digestion
- Increase inflammation
- Disrupt gut health
- Increase cravings for comfort foods
Why Belly Fat Is Often Linked to Stress
Abdominal fat cells are more sensitive to cortisol. Persistent stress increases fat storage in this area, closely linked to insulin resistance and metabolic imbalance.
In such cases, aggressive dieting or intense exercise may worsen the problem by raising stress hormones further.
Scientific Evidence Linking Stress, Sleep, Hormones & Metabolism
| Outcome | Key Finding | Source |
|---|---|---|
| Chronic stress & insulin resistance | Women exposed to chronic stress showed significantly higher abdominal fat and insulin resistance compared to low-stress controls (p ≤ 0.01). |
Aschbacher et al., 2014 PubMed Central |
| Sleep deprivation & metabolic hormones | Sleep debt disrupts leptin, cortisol, growth hormone, and insulin sensitivity, increasing metabolic disease risk. |
Leproult et al., 2009 PubMed Central |
| Poor sleep quality & hormonal imbalance | Disturbed sleep patterns are linked to altered glucose metabolism and lipid regulation through hormonal disruption. |
Kim et al., 2015 PubMed Central |
| Sleep health in women | Midlife women with chronic sleep disturbance show increased metabolic and hormonal health risks. |
Kravitz et al., 2018 PubMed Central |
| Stress & metabolic syndrome | Chronic stress elevates cortisol levels, promoting appetite dysregulation, fat storage, and cardiometabolic risk. |
Rabasa & Dickson, 2016 ScienceDirect |
Non-Food Lifestyle Interventions
- Movement: Walking, yoga, and strength training regulate cortisol and support metabolism.
- Sleep hygiene: Consistent sleep timing and reduced screen exposure improve hormonal rhythms.
- Stress practices: Breathing, journaling, and social connection calm the nervous system.
Consistency matters more than intensity.
Reframing Metabolism: From Control to Support
A stressed body does not respond well to pressure. It responds to safety.
Regular meals, adequate sleep, gentle movement, and emotional support allow cortisol to stabilize. As this happens, insulin sensitivity improves, energy increases, and metabolism begins to regulate.
A More Compassionate Perspective on Women’s Health
- Fatigue is not laziness.
- Cravings are not a lack of discipline.
- Weight gain is not always about overeating.
- Irregular cycles are not random.
These are signals.
Women’s metabolic health is shaped by stress, sleep, emotional load, and hormonal rhythms. Supporting these systems—rather than fighting them—is where true metabolic health begins.
References
- Tsigos C, Chrousos GP. Hypothalamic–pituitary–adrenal axis, neuroendocrine factors and stress. Endocrinology and Metabolism Clinics of North America. https://pubmed.ncbi.nlm.nih.gov/12800539/
- Rosmond R. Stress induced disturbances of the HPA axis: a pathway to abdominal obesity, insulin resistance and cardiovascular disease. Annals of Medicine. https://pubmed.ncbi.nlm.nih.gov/12452869/
- Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. The Lancet. https://pubmed.ncbi.nlm.nih.gov/12531187/
- Fliers E, Kalsbeek A, Boelen A. Beyond the fixed setpoint of the hypothalamus–pituitary–thyroid axis. European Journal of Endocrinology. https://pubmed.ncbi.nlm.nih.gov/30371789/
- Berga SL, Loucks TL. Use of cognitive behavior therapy for functional hypothalamic amenorrhea. Annals of the New York Academy of Sciences. https://pubmed.ncbi.nlm.nih.gov/17978298/
- Foster JA, McVey Neufeld KA. Gut–brain axis: how the microbiome influences anxiety and stress. Trends in Neurosciences. https://pubmed.ncbi.nlm.nih.gov/24720058/
Frequently Asked Questions (FAQs)
- How does stress affect women’s metabolism?
- Chronic stress elevates cortisol, which disrupts insulin sensitivity, promotes abdominal fat storage, and slows metabolic efficiency over time.
- Can stress cause weight gain even without overeating?
- Yes. Elevated cortisol signals the body to conserve energy and store fat, particularly around the abdomen, even when calorie intake is moderate.
- Why does poor sleep worsen hormonal imbalance in women?
- Lack of sleep disrupts cortisol rhythms, increases hunger hormones like ghrelin, reduces insulin sensitivity, and interferes with thyroid function.
- Is belly fat linked more to stress than diet?
- In many women, abdominal fat accumulation is strongly associated with chronic stress and elevated cortisol rather than excess calorie intake alone.
- Can stress affect thyroid function even if blood tests are normal?
- Yes. Chronic stress can impair thyroid hormone activation and cellular response, leading to fatigue and metabolic slowing despite normal lab values.
- What is the best way to support stress-related hormonal imbalance?
- Supporting regular meals, adequate sleep, stress management, gentle movement, and personalised nutrition is more effective than aggressive dieting.
Final Takeaway
Understanding how high cortisol impacts metabolism is crucial for long-term health, especially for women whose hormonal systems are uniquely sensitive to stress. Recognizing the signs and addressing the root causes can help restore balance and improve well-being. Since nutritional needs and stress responses vary widely, exploring DNA-based personalised nutrition offers deeper insights into individual health patterns. For tailored guidance, consider booking a free consultation with unlock.fit to support your metabolic health journey.
Book Your Free Consultation
Share this article
Tavleen
Meet Tavleen, a "human coder" driven by an insatiable passion for genetics that's anything but ordinary. She believes that real change starts at the roots of who we are, and that's precisely why she delved headfirst into the intricate world of Nutrigenomics during her pursuit of a master's degree. But Tavleen's journey doesn't stop there – she's a biohacker extraordinaire, dedicated to unraveling the secrets of how the food we consume can spark astonishing transformations within the tiniest corners of our bodies. Get ready to embark on a captivating exploration of the intersection between genetics, nutrition, and the endless possibilities it holds. Tavleen's unique perspective promises to shed light on the awe-inspiring world of personalised health, and you won't want to miss a single word of her exciting discoveries.