Why Is Bone Health Crucial for Women in India? A Guide to Osteoporosis Prevention

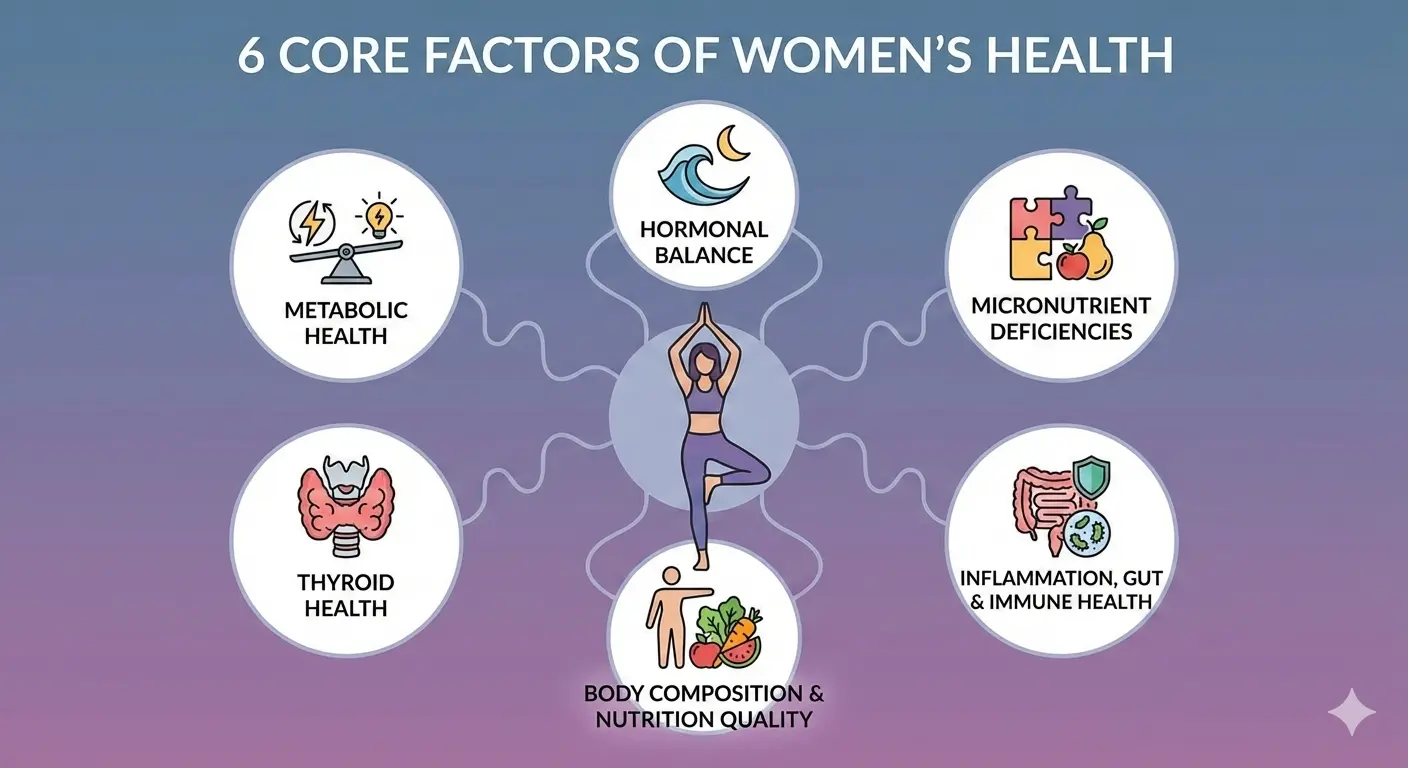
As a clinical dietitian specializing in metabolic health, I often tell my patients that their skeleton is more than just a frame, it is a living, breathing organ that requires constant investment. Yet, in India, we are witnessing a "silent epidemic." Osteoporosis, a skeletal disorder marked by reduced bone density and the deterioration of bone tissue structure, is frequently undiagnosed until it is too late. In our country, the prevalence of this condition peaks 10 to 20 years earlier than in Western nations, creating a significant health and economic burden. For Indian women, the foundation of their future mobility is often under threat long before they realize it. Bone health is not an isolated concern; it is deeply interconnected with hormonal balance, micronutrient status, inflammation, and metabolic health — the same foundations discussed in our guide on the six core factors of women’s health (Place link here to women’s health core factors).
What is the Indian context regarding Vitamin D deficiency and osteoporosis?
India presents a startling health paradox. Despite our geographical location and abundance of sunlight, Vitamin D deficiency is a rampant public health challenge, affecting nearly 70% to 90% of the population. Among Indian women, the statistics are even more sobering. Clinical evaluations of postmenopausal women with Osteoporosis in India show that Vitamin D deficiency (levels <20 ng/mL) is present in a staggering 76% of patients, with another 18% falling into the "insufficient" category.
- The Sunlight Paradox: Even with high UV levels, factors such as high air pollution obstruct Ultraviolet B rays.
- Lifestyle Shifts: Urbanization has led to reduced outdoor activity and increased time spent indoors.
- Cultural Practices: Clothing choices that limit skin exposure and high levels of skin pigmentation can reduce the body's natural synthesis of Vitamin D.
Because bone loss often occurs without symptoms until a fragility fracture happens, many women are unaware they have Osteopenia (low bone mass) until they suffer a minor injury.
Do not rely on "sunny weather" to maintain your Vitamin D status. Given that only 6% of studied Indian women have sufficient levels (>30 ng/mL), a baseline serum test is non-negotiable for anyone over the age of 30, correction of deficiency needs supplementation and dietary changes.Why does timing matter for bone health during menopause?
Understanding bone health requires a shift in how we view time. We must view our bones as a "bone bank" where the most critical deposits are made during our youth.
- The Peak Bone Mass Phase: Bone mineral accretion is most rapid during adolescence, a period that largely predicts the risk of fractures in old age. Reaching a high Peak Bone Mass before the age of 30 is your lifetime insurance policy. However, women face unique biological "withdrawals" during pregnancy and lactation, which are known to result in bone mineral loss from the skeleton.
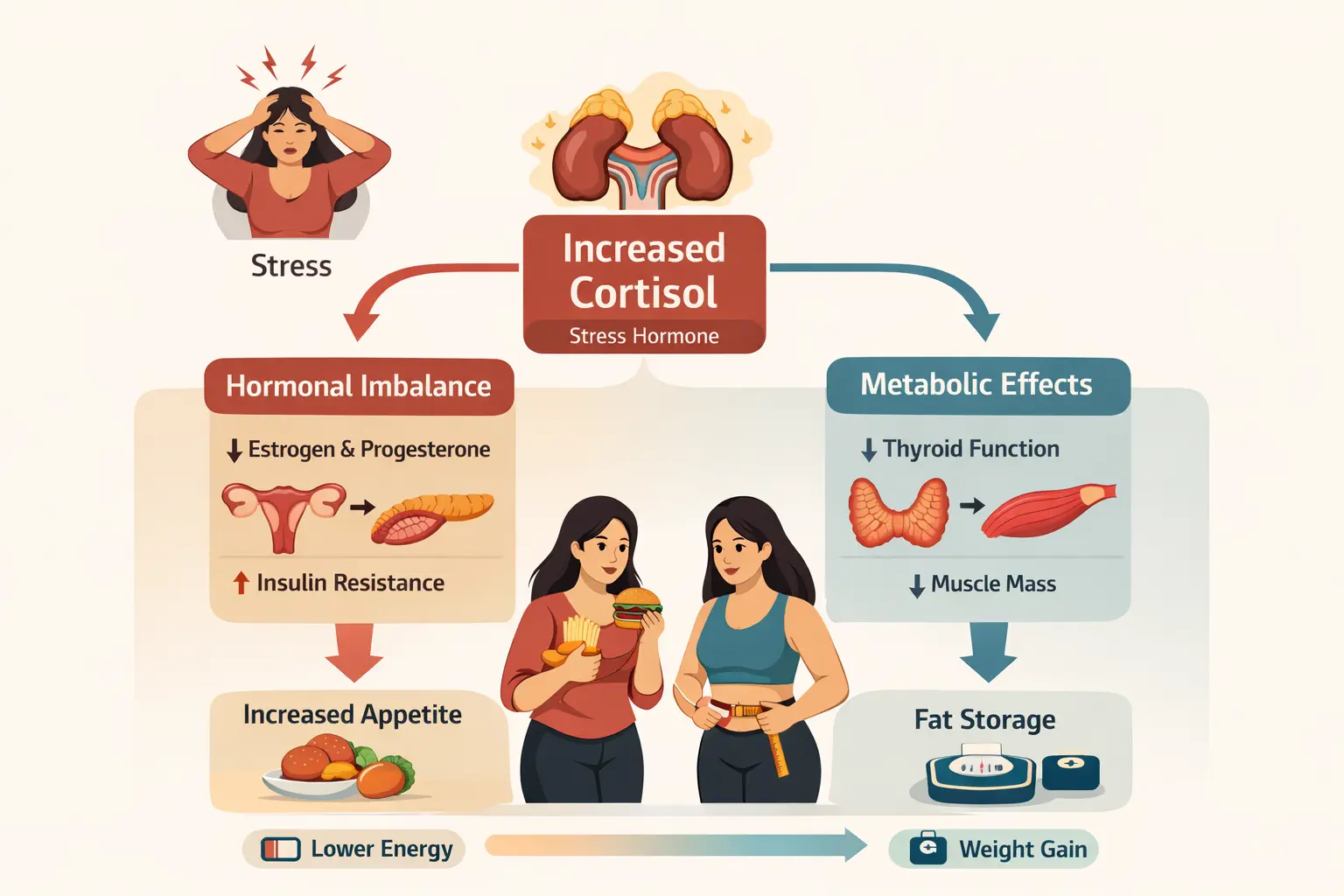
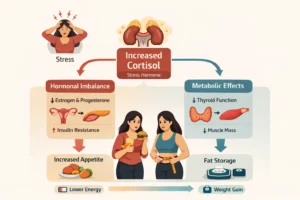
The Physiological Impact of Menopause: The transition into menopause represents the most significant shift in a woman's bone health. During this phase, the cessation of ovarian estrogen production causes a profound hormonal imbalance. Estrogen acts as a protector of the skeleton; when levels drop, the body moves into a state where bone Resorption (breakdown) significantly outweighs bone formation. This acceleration of skeletal demineralization makes perimenopausal and postmenopausal women a high-risk group.
The decade following menopause is when you can lose the most bone density. If you are entering this phase, it is vital to discuss your "bone turnover" markers and protective strategies with a clinical dietitian or healthcare provider immediately.
What are the risk factors that influence your bone health?
Bone health is influenced by a complex matrix of factors, some modifiable and others determined by biology.
- Lifestyle Triggers
- Dietary Gaps: Inadequate intake of calcium and Vitamin D results in alterations in bone structure and strength.
- Sedentary Behavior: A lack of weight-bearing physical activity is a primary modifiable risk factor for decreased mineral density.
- The "Salt" Factor: Interestingly, clinicians observe that higher dietary sodium (salt) intake is associated with negative calcium balance, bone mineral loss, and an increased risk of fracture.
- Caffeine and Soft Drinks: Regular intake of carbonated soft drinks and high caffeine consumption are linked to decreased calcium absorption.
- Biological Triggers
- Genetic Predisposition: Factors beyond your control, such as a family history of Osteoporosis, play a significant role.
- BMI and Body Composition: A low Body Mass Index (BMI) (e.g., <19 kg/m²) is a significant risk factor for reduced bone density.
- Thyroid dysfunction also plays a crucial role, as exlained in our recent blog on thyroid dysfunction and bone health where slowed metabolism and hormonal imbalance can indirectly weaken skeletal strength.
- Early Menopause: Women who experience menopause early have a longer duration of estrogen deficiency, leading to a weak inverse correlation where longer menopause duration is associated with lower Vitamin D levels.
- Chronic Metabolic Dysfunction such as Insulin resistance contributes to systemic inflammation, which can accelerate bone degradation and impair calcium metabolism.
Audit your kitchen for hidden salt. High sodium intake increases calcium excretion in the urine, effectively "flushing" your bone-building blocks away.
How do calcium and Vitamin D work together for bone strength?
In clinical nutrition, we focus on the biological "partnership" between minerals and vitamins. You cannot build a foundation with bricks alone; you need mortar.
Calcium is the foundational mineral for bone strength. However, Vitamin D is essential for calcium-phosphorus homeostasis. Its primary role is to enhance the intestinal absorption of calcium.
When Vitamin D is deficient, this axis is disrupted, leading to:
- Hypocalcemia: Low total serum calcium levels (noted in 58% of studied osteoporotic women).
- Secondary Hyperparathyroidism: The body compensates for low Vitamin D by increasing Parathyroid Hormone (PTH), which triggers bone Resorption to maintain blood calcium levels.
- Fragility Fractures: Women with low Vitamin D exhibit significantly lower mineral levels and a higher history of fractures (13.8 ng/mL vs. 17.9 ng/mL in those without fractures).
Taking a calcium supplement without checking your Vitamin D is like pouring water into a bucket with a hole in the bottom. Vitamin D is the plug that helps your body retain and use that calcium.
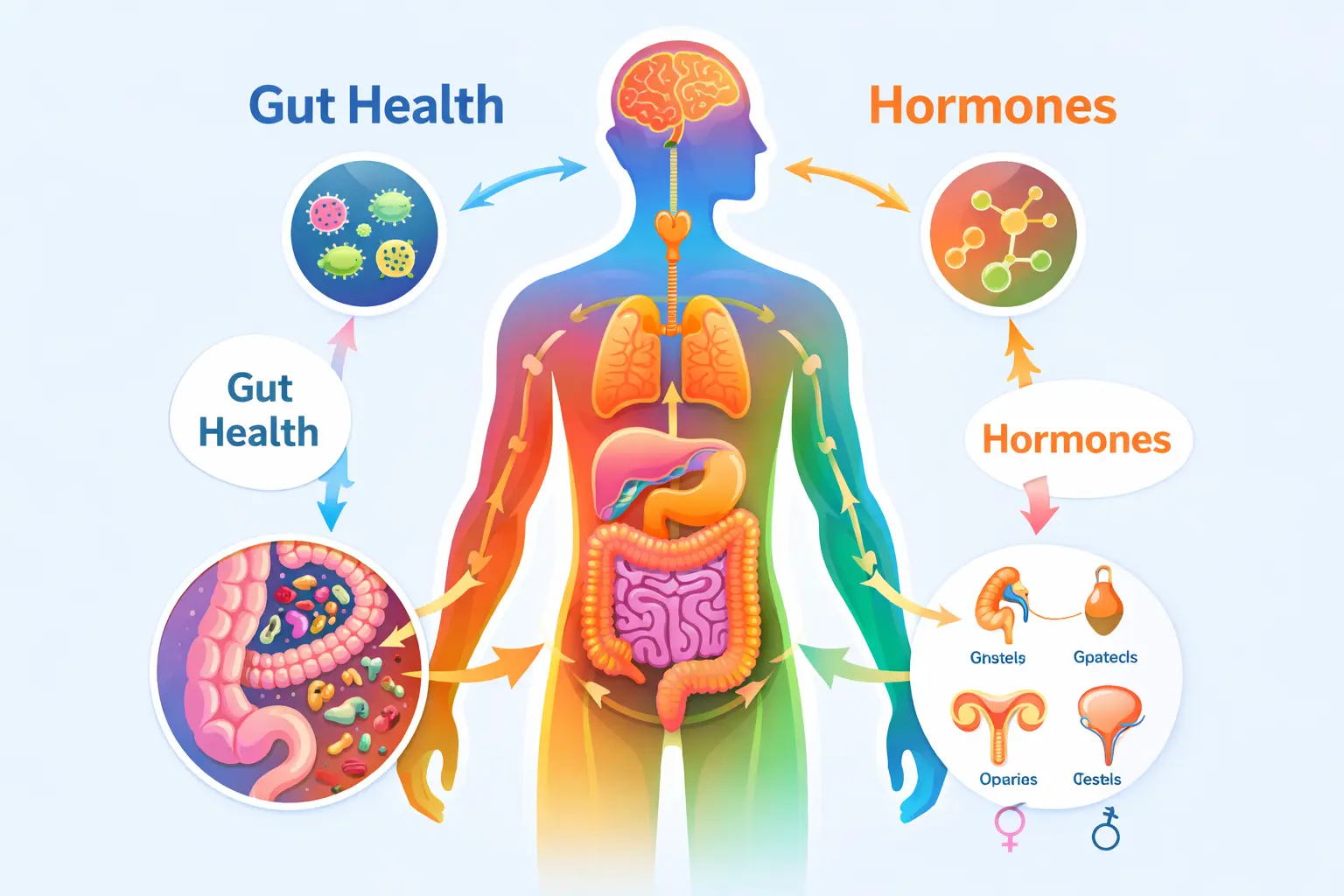
Calcium absorption and Vitamin D metabolism are also influenced by gut health and hormone regulation, as microbiome imbalances can impair nutrient absorption and inflammatory balance.
What role does nutrigenomics play in understanding bone health?
Recent advances in Nutrigenomics allow us to identify high-risk individuals before symptoms appear. Genetic factors may account for 23% to 80% of the variability in serum Vitamin D levels.
One of the most important genetic variants is the VDR (Vitamin D Receptor) gene. Specific polymorphisms, such as the BsmI polymorphism (rs1544410), influence how your body responds to Vitamin D and its effect on bone mineral density.
Genotype Influence: Studies have identified different genotypes (TT, TC, CC). In some populations, those carrying the "T" allele may have a higher risk of developing Vitamin D deficiency compared to others.
Personalized Approach: Identifying these variants helps clinicians design tailored nutritional approaches to prevent or delay the development of Osteoporosis.
This is where DNA-based personalized nutrition for Indian women becomes valuable, allowing targeted correction of Vitamin D receptor variations and calcium metabolism differences.
How can you measure your bone health through diagnostics and screening?
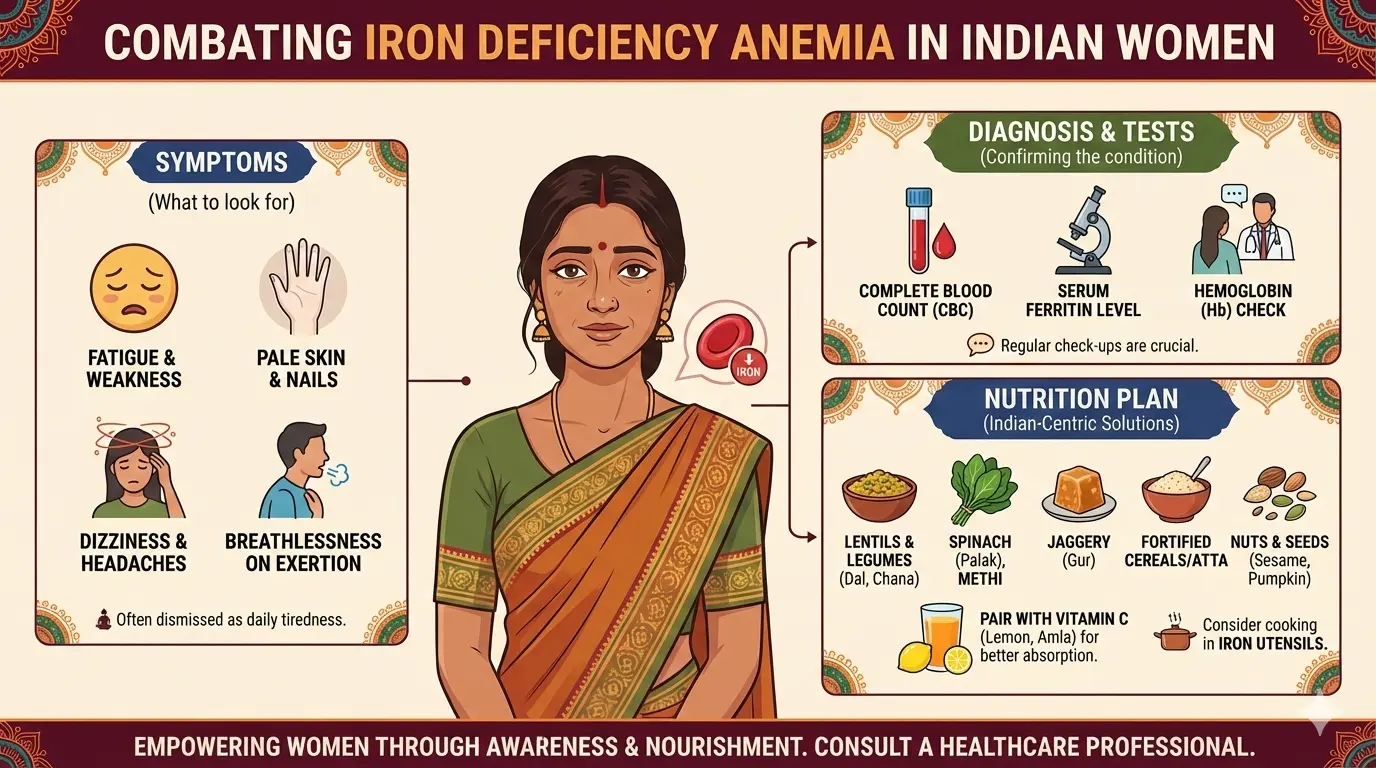
To manage your bone health, you must measure it. I recommend three critical blood markers and one gold-standard scan.
Key Blood Markers
| Marker Name | Normal/Optimal Range | Why it matters for Bone Health |
|---|---|---|
| Serum 25(OH) Vitamin D | Deficiency: <20 ng/mL Insufficient: 20–30 ng/mL Optimal: 30–50 ng/mL | Required for calcium absorption and bone mineralisation. Low levels increase fracture risk. |
| Total Serum Calcium | 8.5 – 10.5 mg/dL | Reflects circulating calcium levels. Low levels may indicate poor intake, malabsorption, or Vitamin D deficiency. |
| Parathyroid Hormone (PTH) | 10 – 65 pg/mL | Elevated PTH suggests secondary hyperparathyroidism due to Vitamin D deficiency, leading to bone resorption. |
| Magnesium | 1.7 – 2.2 mg/dL | Supports Vitamin D activation and bone matrix stability. |
| Phosphorus | 2.5 – 4.5 mg/dL | Works with calcium in bone mineral structure. |
The DEXA Scan
The DEXA Scan (Dual-Energy X-ray Absorptiometry) is the gold standard for measuring bone mineral density (BMD). It provides a T-score, which compares your bone density to that of a healthy young adult:
- Normal: -1.0 or higher.
- Osteopenia: -1.0 to -2.5.
- Osteoporosis: -2.5 or lower.
T-score of -2.5 is very common in postmenopausal Indian women. Do not wait until your score is in the danger zone to start dietary interventions.
What is the Indian bone-health protocol for nutrition and exercise?
Based on clinical evidence, preventing bone loss requires a dual approach of specific nutrients and physical "pressure" on the bones.
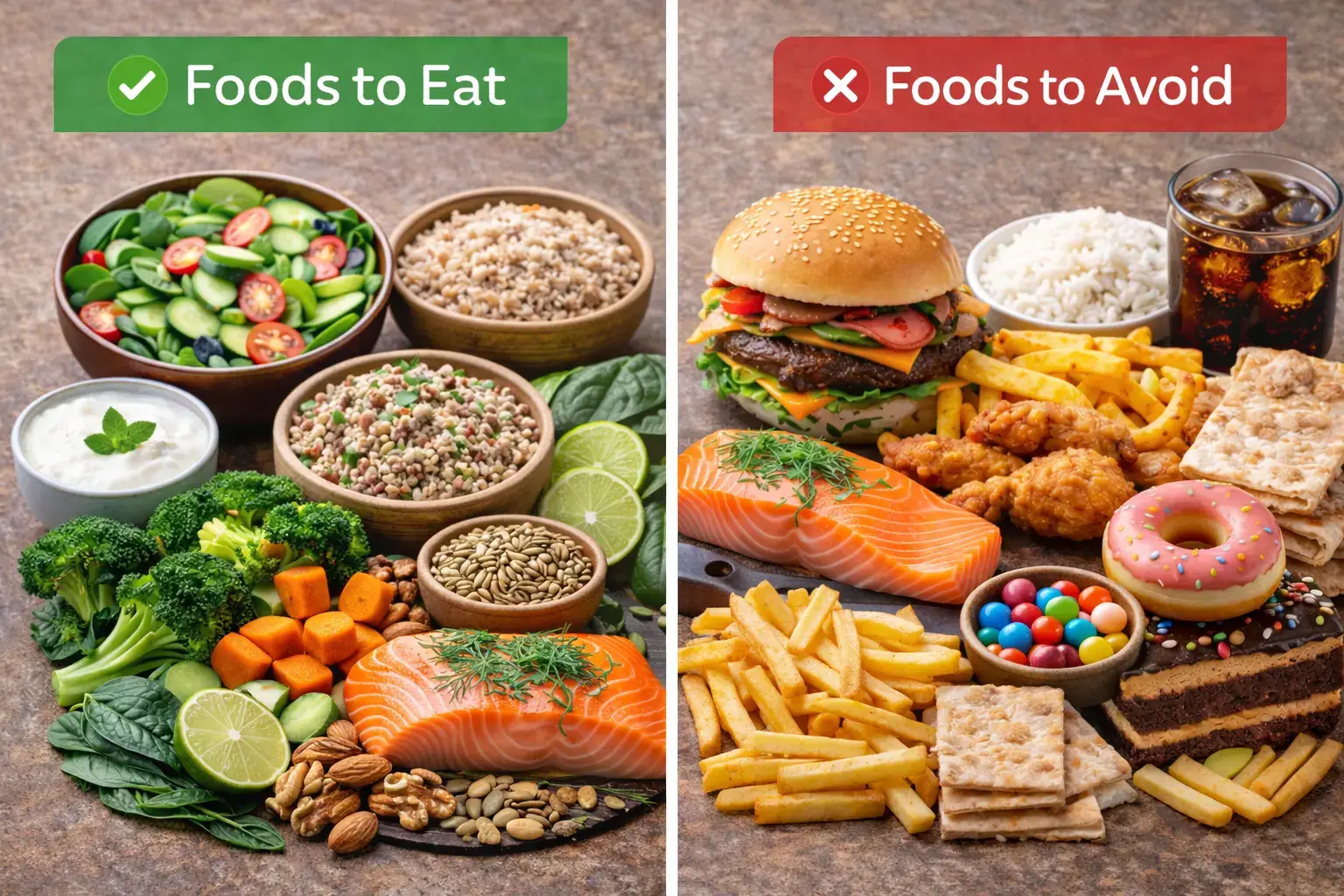
Dietary Action Steps: Beyond Dairy: While dairy is a potent source of calcium, a diverse diet is essential for bone mineralization.
- Dairy Sources: Milk, cheese, and yogurt are the most beneficial dairy products for bone health.
- Non-Dairy Calcium: Incorporate almonds and green leafy vegetables (like spinach), millets like ragi (finger millet) into your daily meals.
- Vitamin K2: Often missing from the Indian diet, Vitamin K2 is the "traffic cop" that ensures calcium goes into the bones rather than the arteries. It is found in fermented foods like Natto (fermented soy), green leafy vegetables, cheese, egg yolks.
- The Supporting Cast: Ensure adequate intake of Magnesium and Protein, which are emerging as critical components for improving bone structure and density.
- Preferred Supplements: In clinical settings, organic calcium like calcium aspartate anhydrous is often preferred for better absorption, bioavailability, and gastrointestinal tolerability.
| Food Source | Approx Calcium/Serving | Vitamin K2 |
|---|---|---|
| Milk (1Cup) | 240-300mg | Low |
| Curd/Yogurt (1 Cup) | 200-250 mg | Moderate |
| Ragi (100g) | 35-400 mg | Minimal |
| Spinach (1 Cup cooked) | 120 mg | Low |
| Almonds (30g) | 75-80 mg | Minimal |
| Cheese (30g) | 200 mg | Moderate |
| Egg Yolk (1 Large) | 22 mg | Moderate |
| Fermented Soy (100 mg) | 380 mg | 1500 mcg |

How does high salt intake affect your bone density?
One of the most significant findings in recent Indian clinical surveys is the impact of dietary sodium (salt). High salt intake is a major contributor to a negative calcium balance.
Mechanism: Excessive sodium consumption increases calcium excretion in the urine. Essentially, the more salt you eat, the more calcium your body "flushes out," leading to bone mineral loss even if your calcium intake is high.
Clinicians have found that this salt-driven mineral loss significantly elevates the risk of fractures.
Protein Synergy: Adequate protein is necessary for the collagen matrix of the bone. Without protein, the "bricks" of calcium have no structure to hold onto.
Why is clinical supplementation important for bone health?
If diet alone is insufficient, which is the case for 76% of deficient women, supplementation is required.
Preferred Calcium Salts: Many Indian experts now prefer Calcium Aspartate Anhydrous over traditional calcium carbonate.
Why Aspartate? This organic form offers better absorption, higher bioavailability, and superior gastrointestinal tolerability, meaning it is less likely to cause the bloating or constipation often associated with cheaper supplements.
How can sunlight exposure and fortification strategies improve Vitamin D levels?
Awareness of sunlight is high (83%), but the implementation is low due to air pollution and indoor lifestyles.
Safe Sun Exposure: Aim for mid-day exposure when UVB rays are highest, but recognize that in high-pollution cities, this may not be enough.
Fortification: Emerging solutions like fortified milk have shown success in improving serum Vitamin D levels in Indian pilot studies.

What dietary action steps can you take to enhance bone health?
Dietary Action Steps Checklist:
| Action Steps | Why It Matters |
|---|---|
| Reduce Salt Intake | High sodium increases urinary calcium loss |
| Ensure Vitamin D Testing | Prevents silent deficiency |
| Diversify Calcium sources | Improves overall mineral intake |
| Add Fermented Foods | Supports Vit K2 & gut health |
| Include Weight Bearing Exercise | Stimulates bone formation |
| Maintain Adequate Protein | Supports collagen bone matrix |
| Limit Carbonated Drinks | Reduces calcium depletion |
Most adults typically take only 0.5 mg to 2.0 mg of calcium per day, which is far below the recommended levels. To fix this, don't just "eat more" eat smarter by combining your calcium intake with Vitamin D and magnesium while cutting back on hidden salt in processed snacks.
How can exercise contribute to stronger bones?
Bones are living tissues that grow stronger when they are challenged.
- Weight-Bearing Exercise: Activities where you move against gravity. Brisk walking and slow exercises are highly recommended.
- Resistance Training: This involves using weights or bodyweight to improve bone density, which is particularly effective for postmenopausal women.
- Balance and Flexibility: Yoga and swimming are excellent for maintaining muscle strength and balance, which significantly reduces the risk of falls—the leading cause of fractures in the elderly.
Combine your weight-bearing exercise with sun exposure. A 20-minute morning walk provides the mechanical stress your bones need and the UV exposure your skin requires for Vitamin D synthesis.
How can you take charge of your bone health foundation?
Osteoporosis is a preventable ailment, but the first step is awareness of your personal risk factors. Given that nearly 50% of postmenopausal women with fractures in India have severe Vitamin D deficiency, the time for passive observation is over.
Check your markers, understand your genetic blueprint, and invest in your "bone bank" today. Your future mobility depends on the foundation you build right now.
Consultation with a healthcare provider is essential before starting any new supplement or exercise regimen to ensure it is appropriate for your specific health profile.
What common questions do women have about osteoporosis and bone health?
- Why is osteoporosis a bigger concern for Indian women compared to those in the West?
In India, the prevalence of osteoporosis reaches its peak 10 to 20 years earlier than in Western nations. This earlier onset is often linked to the "silent epidemic" of Vitamin D deficiency, which affects nearly 70% to 90% of the Indian population. Specifically, among postmenopausal women with osteoporosis in India, clinical studies show that 76% are deficient in Vitamin D (<20 ng/mL) and 58% suffer from hypocalcemia (low serum calcium). This unique Indian context driven by high air pollution obstructing UVB rays, indoor lifestyles, and skin pigmentation means our "bone bank" often depletes much faster than that of our global peers.
- How does my salt intake affect my bone density?
Many women are surprised to learn that their salt shaker is a "silent thief" of bone mineral density. Clinical studies indicate that high dietary sodium (salt) intake is significantly associated with a negative calcium balance and bone mineral loss. When you consume excessive salt, your body compensates by increasing calcium excretion in the urine. Essentially, the more salt you eat, the more calcium your body "flushes out" instead of using it to strengthen your bones. This makes managing sodium intake just as critical as increasing calcium intake for preventing fractures.
- Can my genetics really determine my risk for osteoporosis?
Yes. While diet and lifestyle are modifiable, your genetic blueprint accounts for 23% to 80% of the variability in your serum Vitamin D levels. A specific variation in the Vitamin D Receptor (VDR) gene, known as the BsmI polymorphism, significantly influences how your body processes Vitamin D. Some studies suggest that individuals carrying certain mutant alleles may have twice the risk of developing Vitamin D deficiency compared to those with the reference genotype. Understanding your genetic predisposition allows for "personalized medicine," where we can tailor your nutrient intake to overcome genetic absorption hurdles.
- I don’t consume much dairy; what are my other options for bone health?
Awareness of non-dairy calcium is a major gap; only 37% of women in some surveys could correctly identify calcium-rich food sources. Beyond milk, you should focus on Ragi (finger millet), almonds, seeds, and green leafy vegetables like spinach. For those requiring supplementation, many Indian clinicians now prefer calcium aspartate anhydrous over traditional salts because it offers better absorption, higher bioavailability, and superior gastrointestinal tolerability. Additionally, ensure you are getting Vitamin K2 (found in fermented foods like Natto, egg yolk, cheese) and Magnesium, which are essential for directing calcium into the bone matrix.
Final Takeaway
Bone health is a critical aspect of overall well-being, especially for Indian women who face unique challenges due to cultural and environmental factors. By understanding the importance of Vitamin D, calcium, and other nutrients, and by adopting a proactive approach to diet, exercise, and lifestyle, women can significantly reduce their risk of osteoporosis and maintain strong, healthy bones throughout their lives.
Book Your Free Consultation
Share this article
Nihala Ibrahim
Nihala Ibrahim is a clinical dietitian with a scientific approach to personalized nutrition and metabolic health. She passionately bridges clinical insights with evidence-based diet strategies to help clients overcome diabetes, thyroid issues, PCOS, and weight challenges for optimal wellness. She holds Masters in clinical dietetics and nutrition science from Sri Ramachandra Institute, Chennai.