How to Manage PMS: Diet Plans, Hormone Testing Recommendations and Lifestyle Changes for Relief

What Is a “Normal” Menstrual Cycle and How Is It Defined?
As a Clinical Dietitian, I have sat across from countless women who believed that debilitating pain, explosive mood swings, and crushing fatigue were simply the "price of being a woman." We have been conditioned to accept suffering as a standard part of our monthly rhythm. I am here to tell you that while PMS symptoms are incredibly common, they are not necessarily normal.
There is a profound difference between a minor "physiological" nudge from your body and a "pathological" scream for help. When your cycle is consistently characterized by severe symptoms, it is often a messenger signaling an underlying metabolic or hormonal imbalance, such as Polycystic Ovary Syndrome (PCOS), thyroid dysfunction, or endometriosis. My goal today is to help you translate those messages and harness the power of personalized nutrition to reclaim your health.
To understand when things are off, we first need to define the baseline. In clinical terms, we often refer to the menstrual cycle as a "vital sign," much like your blood pressure or heart rate.
- Cycle Length: A typical, healthy cycle lasts between 21 and 35 days. While some variation is natural, cycles that consistently fall outside this window either too short or too long—are considered "irregular" and warrant investigation.
- The Flow: The average duration of menstrual flow is approximately 2 to 8 days.
- Manageable Symptoms: A "normal" period might involve mild cramping that responds to gentle movement or heat, and perhaps a slight shift in energy. It should not, however, interfere with your ability to go to work, attend school, or maintain your relationships.
Irregularity is more than just an inconvenience; it is often a sign of disrupted follicular development or hormonal signaling. For instance, adolescents and young adults who skip breakfast or face extreme nutritional stress are significantly more likely to experience irregular cycles.
What Are the Common Symptoms of PMS and Period Pain?
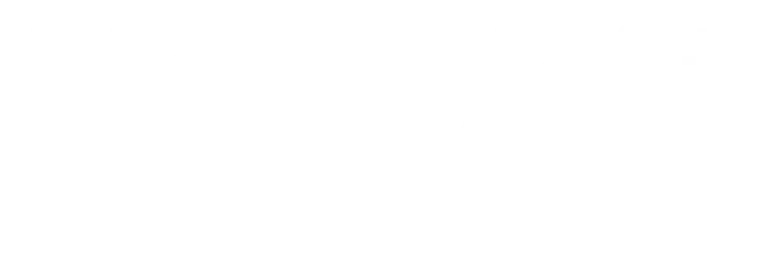
Premenstrual Syndrome (PMS) is a constellation of symptoms that occur during the luteal phase (the time between ovulation and your period) and resolve once your flow begins. Studies among young women show a staggering prevalence of nearly 67%, with many experiencing moderate to severe symptoms.
The Physical Impact
The physical side of PMS often feels like a full-body inflammatory event. Key symptoms include:
- Pelvic Pain and Abdominal Cramps: These are the most frequently reported physical complaints, often leading women to rely on painkillers to get through the day.
- Bloating and Weight Gain: Often driven by sodium-induced fluid retention.
- Breast Tenderness and Swelling: A common sign of hormonal shifts affecting fluid balance.
- Headaches and Fatigue: Often linked to inflammatory markers and fluctuations in blood sugar.
The Emotional Rollercoaster
The psychological symptoms of PMS can be even more disruptive than the physical ones. Many women report:
- Irritability and Mood Swings: These are core features of emotional instability during the luteal phase.
- Anxiety and Low Mood: Feelings of depression or tension that seem to vanish once the period starts.
- Loss of Concentration: A brain-fog sensation that can impair academic or professional work performance.
When Should You Consider Testing Your Hormones?
If your symptoms fall into the "severe" category, we need to look under the hood. Hormones do not work in a vacuum; they are deeply influenced by your metabolic health and lifestyle.
PCOS and the Insulin Resistance Link
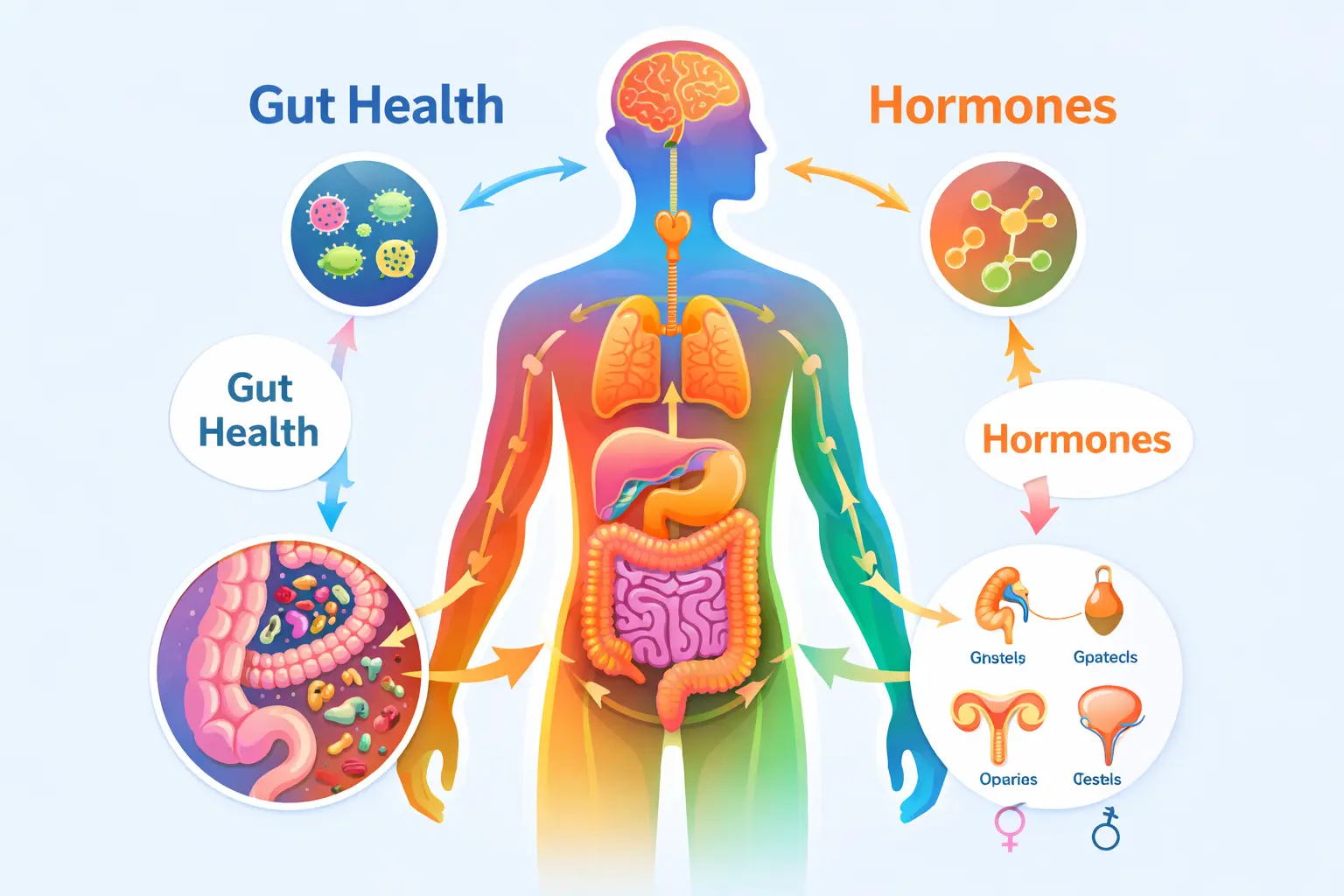
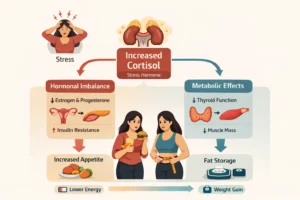
Polycystic Ovary Syndrome (PCOS) is increasingly common, often linked to the "triple burden" of malnutrition we see today specifically overnutrition or excess caloric intake. The hallmark of PCOS is often Insulin resistance , where your body’s cells don't respond well to insulin, leading to higher levels of both insulin and sugar in the blood.
We see a clear correlation between high consumption of Ultra-Processed Foods (UPFs) and increased visceral fat (fat stored around your internal organs). This excess adiposity (fat tissue) acts like its own endocrine organ, pumping out inflammatory signals that disrupt your cycle and worsen PMS symptoms.
Thyroid Dysfunction (Hypo/Hyper)
Your thyroid is your body’s metabolic thermostat. If it is underactive (Hypothyroidism) or overactive (Hyperthyroidism), it can cause cycles to become extremely heavy, infrequent, or stop altogether. Thyroid health is a foundational pillar of regular menstruation.
Endometriosis and Fibroids
These conditions are characterized by abnormal tissue growth—either uterine-like tissue growing outside the uterus (endometriosis) or non-cancerous growths within the uterus (fibroids). Both are heavily influenced by inflammation and hormonal imbalances, often leading to severe pelvic pain and heavy bleeding.
Lifestyle Stressors: Stress, RED-S, and Over-exercising
Your body is designed for survival. If it perceives a threat—whether that is the "threat" of a looming deadline or the "threat" of not having enough food—it may shut down "non-essential" functions like reproduction.
- RED-S (Relative Energy Deficiency in Sport): This occurs when your energy intake doesn't match your energy expenditure. It is a form of undernutrition that can lead to delayed menarche (the first period) or the loss of a cycle (amenorrhea).
- Over-exercising: While movement is vital, excessive intensity without proper recovery can spike cortisol (the stress hormone), which directly competes with your sex hormones.
How Can Diet Help in Reducing PMS and Pain?
I always tell my clients: "Test, don't guess." You should consider clinical testing if you experience "Red Flag" symptoms, such as:
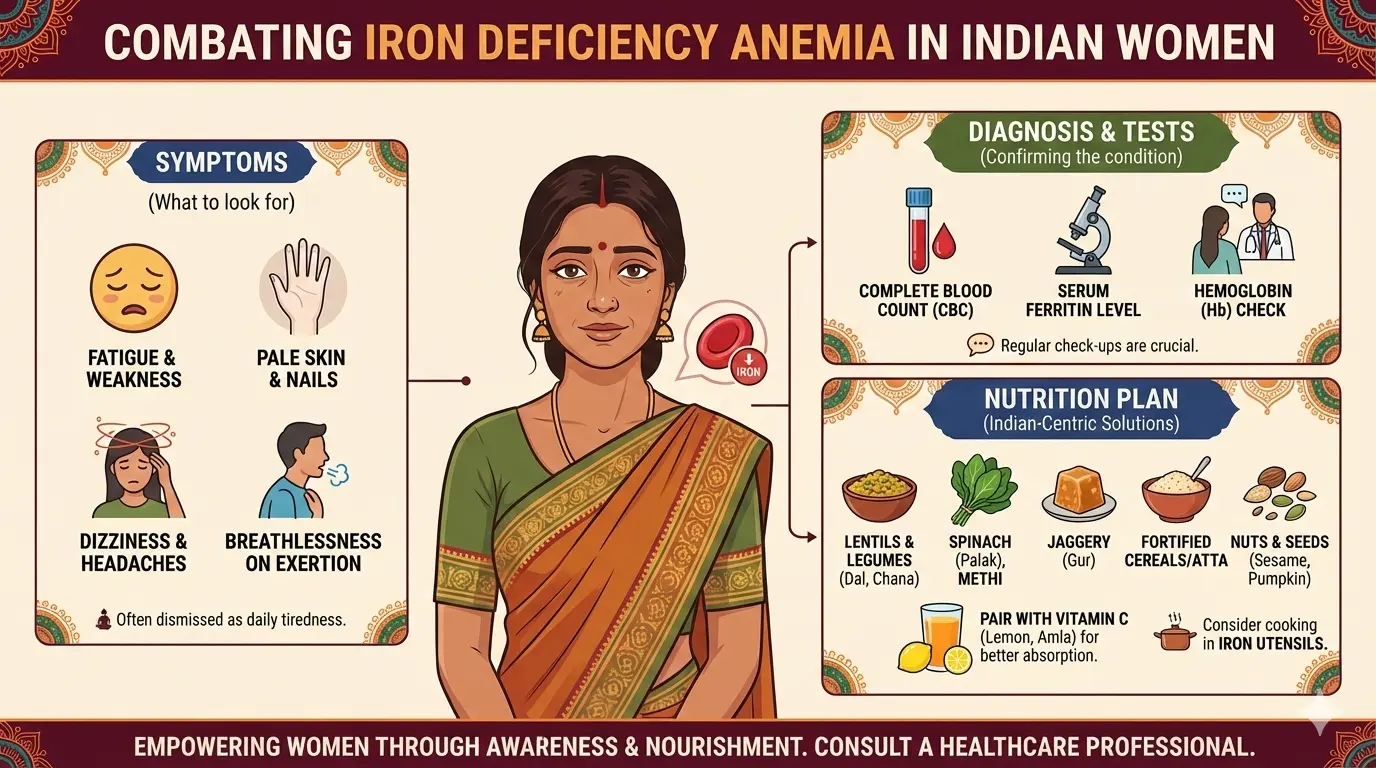
- Heavy bleeding that requires changing a pad or tampon every hour (which increases your risk for iron deficiency anemia).
- Severe pain that doesn't respond to standard over-the-counter interventions.
- Infertility or inability to track an ovulatory window.
- Cycles consistently shorter than 21 days or longer than 35 days.
Common tests include a Thyroid profile (TSH, T3, T4), an LH/FSH ratio (often used to screen for PCOS), Prolactin, Androgens (male-pattern hormones like testosterone), and a pelvic Ultrasound to check for cysts or fibroids.
Why Is It Important to Reduce Sugar and Refined Carbs?
The strongest nutritional link to PMS relief lies in managing your intake of pro-inflammatory foods. Research consistently shows a statistically significant correlation between high consumption of refined sugars and salty foods and increased PMS severity. Refined sugars cause rapid glycemic spikes and crashes, which destabilize your mood and disrupt serotonin regulation. Similarly, high salt intake triggers the renin-angiotensin-aldosterone system, leading to the bloating, breast tenderness, and headaches many experience during the luteal phase.
Diets high in refined sugars (sweets, biscuits, cakes) and salty foods (chips, processed snacks) are significantly correlated with more severe PMS.
- Glycemic Spikes: Refined sugars cause rapid spikes in blood glucose followed by sharp crashes. This volatility intensifies mood swings, irritability, and fatigue.
- Serotonin Disruption: These sugar crashes can disrupt serotonin, the "feel-good" neurotransmitter. Lower serotonin in the luteal phase leads to the classic cycle of carbohydrate cravings and worsening mood.
How Do Whole Foods and Omega-3s Benefit PMS Relief?
Colorful Vegetables: These provide the fiber needed for healthy bowel movements, which is crucial because your body "poops out" excess estrogen. Low fiber intake is directly linked to bloating and unsatisfactory digestion.
Omega-3 Fatty Acids: Found in fatty fish like salmon or seeds like flax, these are powerful anti-inflammatories that can help dampen the "cramp" signals in your pelvis.
Whole Grains: These provide steady energy and B-vitamins, helping to avoid the glycemic roller coaster.
Which Key Nutrients Support a Healthy Menstrual Cycle?
| Nutrients | Role in Women’s Health | Addition Notes |
|---|---|---|
| Magnesium | Supports mood regulation and muscle relaxation | Commonly deficient in individuals consuming high-sugar diets |
| Vitamin B6 | Helps relieve PMS symptoms and supports neurotransmitter synthesis | Found in bananas, potatoes, and other whole foods |
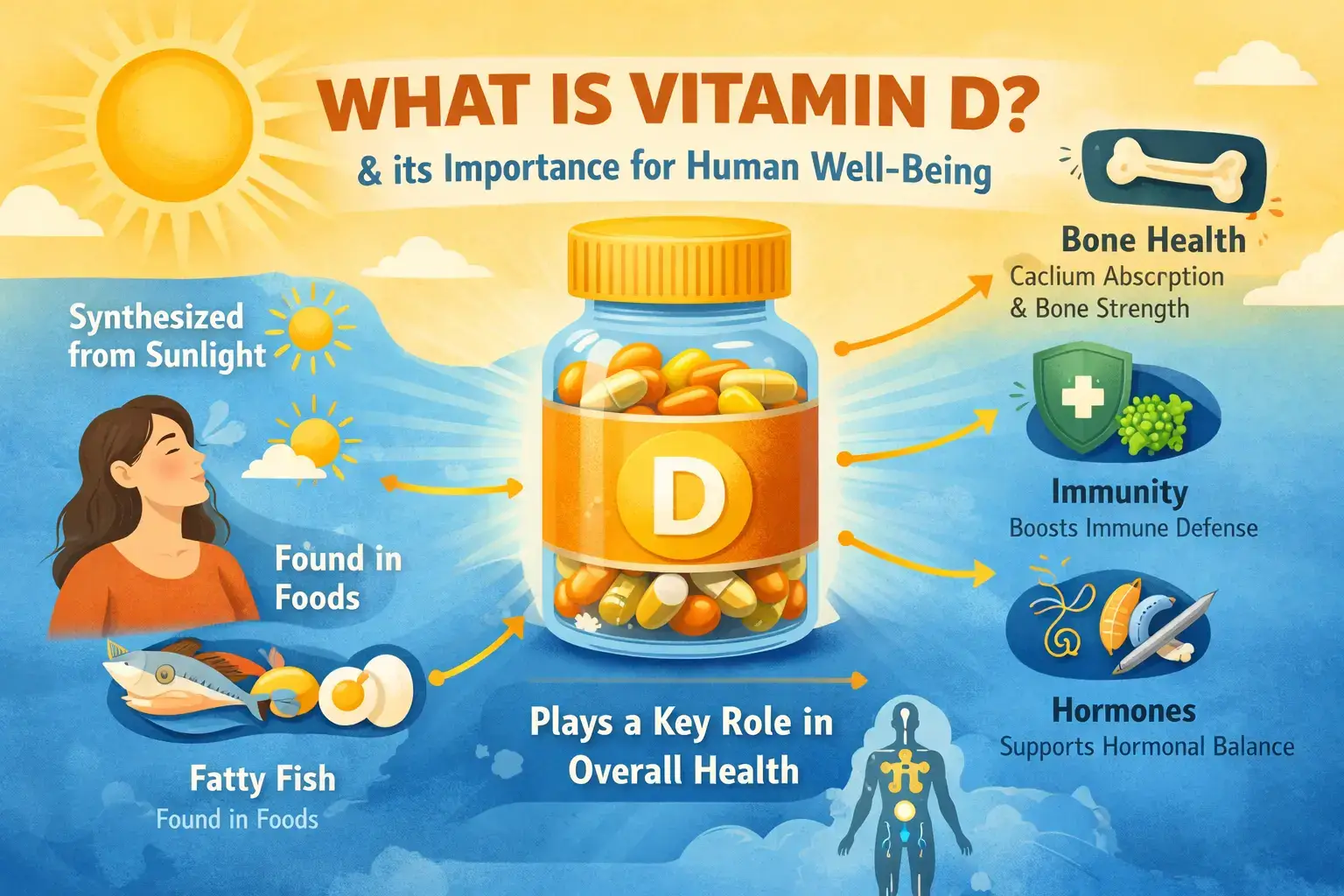
| Calcium and Vitamin D | Regulate cellular electrical activity and support mood stability | Vitamin D deficiency affects up to 80% in some populations; linked to low bone density and higher autoimmune risk |
Why Is Meal Consistency Key to Managing PMS Symptoms?
One of the most overlooked strategies for PMS relief is meal consistency. Studies have identified a significant positive association between meal skipping and the intensity of PMS symptoms. Habitual meal skippers—particularly those who skip breakfast—report more irregular and painful periods. Skipping meals exacerbates micronutrient deficiencies in zinc, iron, and B vitamins, which are vital for maintaining the hormonal equilibrium required for a smooth cycle.
How Do DNA and Blood Tests Inform Period Health?
In my practice, I use a two-pronged approach to data:
- DNA Markers (The Blueprint): Your genetic makeup can tell us if you have a predisposition for higher inflammation or insulin resistance. Think of this as the "architect’s plan" for your body it tells us what might happen.
- Blood Tests (The Status Report): Blood tests tell us what is happening right now.
- Iron/Hemoglobin: To check for anemia, which causes the hallmark PMS symptom of fatigue.
- Vitamin D: To ensure you have the hormonal building blocks you need.
- CRP (C-Reactive Protein): A marker of systemic inflammation.
- Insulin: To check for metabolic flexibility and insulin resistance.
- Thyroid profile (TSH, T3, T4)
By combining these, we can personalize your diet. For example, if your "status report" shows high insulin, we prioritize low-glycemic foods immediately.
Please also read our recent blog on 11 Blood Tests that Reveal Your Metabolic Health.
What Lifestyle Habits Can Improve Menstrual Cycles?
Nutrition is the foundation, but lifestyle habits provide the structure.
| Lifestyle Habit | Key Impact on Hormones | Evidence / Notes |
|---|---|---|
| Circadian Rhythm (Sleep) | Stabilizes hormonal rhythms and reduces stress response | 6 to 8 hours of regular sleep is associated with lower PMS severity |
| Strength Training | Improves body composition and supports hormonal balance | Increases lean muscle mass and helps manage visceral fat, better indicator than BMI |
| Stress Management | Reduces cortisol and PMS severity | Mindfulness and moderate activity reduce stress-related hormonal disruption |
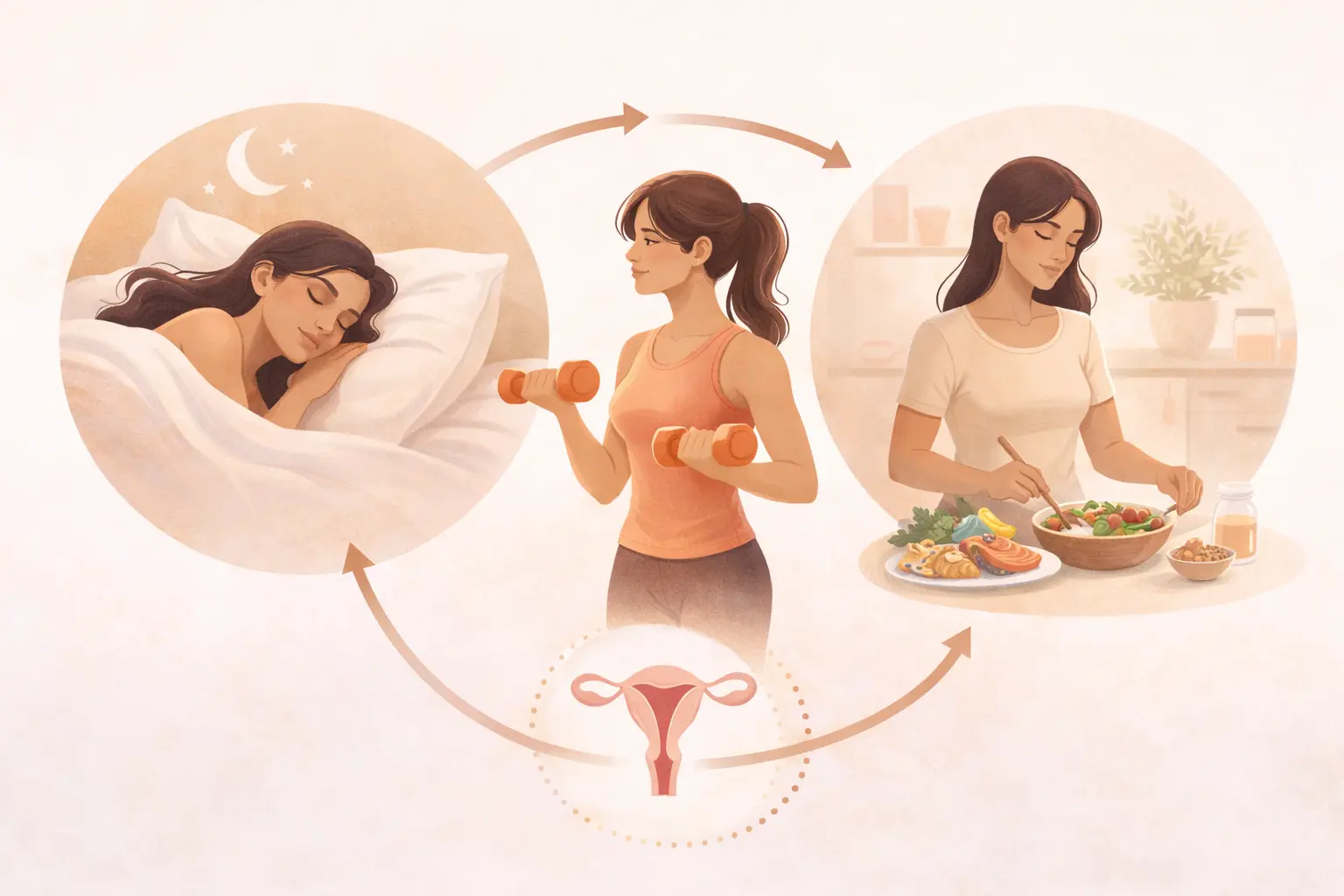
In my clinical experience, I often describe sleep as a non-negotiable pillar of hormonal health. Research highlights a statistically significant negative correlation between adequate sleep duration and the severity of Premenstrual Syndrome (PMS) symptoms. Specifically, individuals who consistently achieve 6–8 hours of sleep per day report significantly lower PMS severity compared to those with irregular or shorter rest periods.
This connection is deeply physiological, as adequate sleep helps stabilize hormonal rhythms and mitigates the body's stress response, both of which are critical for managing premenstrual distress. Conversely, sleep disorders are a common clinical feature among women with reproductive endocrine disorders, illustrating the bidirectional link between rest and reproductive function. Modern lifestyle stressors, such as excessive screen exposure, further threaten this balance by reducing total sleep time and reinforcing sedentary behaviors.
Ultimately, prioritizing sleep hygiene serves as a powerful, cost-effective, and non-pharmacological intervention to reduce symptom intensity. Recognizing sleep as a modifiable lifestyle factor is essential for any woman seeking to reclaim her cycle health and improve her long-term metabolic well-being.
What Are Common Questions About PMS and Period Pain?
-
Q.1. My periods are very painful and my moods are all over the place. Is this just a "normal" part of being a woman?
Answer: While symptoms like mild cramping and mood shifts are incredibly common affecting between 30% and 80% of women—they are not necessarily normal if they disrupt your life. A healthy cycle typically lasts 21 to 35 days, with bleeding for about 2 to 8 days. If your pain requires heavy medication to function, or if your "mood swings" (emotional instability) interfere with your relationships and work, your body may be signaling an underlying issue. Severe symptoms can sometimes be linked to conditions like PCOS, thyroid dysfunction, or deeper metabolic imbalances. These are part of the broader core factors that influence women’s hormonal health, and they require clinical investigation rather than just "toughing it out". Q.2. How much does what I eat actually affect my cramps and bloating?
Answer: Your diet plays a massive role in the intensity of your symptoms. Research shows a significant positive correlation between the consumption of refined sugars and salty foods and the severity of PMS. High sugar intake causes rapid "spikes and crashes" in blood glucose, which can worsen irritability, fatigue, and mood swings. Meanwhile, excess salt triggers fluid retention, leading to bloating, breast tenderness, and headaches. Additionally, a heavy reliance on Ultra-Processed Foods (UPFs) is linked to increased visceral fat (fat around internal organs), which can further disrupt your hormonal balance and metabolic health. Q.3. I often skip breakfast or forget to eat when I’m busy. Could this be making my PMS worse?
Answer: Yes, absolutely. Habitual meal skipping, particularly breakfast, is a known predictor of irregular and more painful periods. When you skip major meals, you are more likely to develop micronutrient deficiencies in vitamins and minerals like Magnesium, Zinc, and Vitamin B6, which are essential for stabilizing your mood and clearing out excess hormones. Clinical data shows that women who frequently skip meals report higher levels of psychological distress, such as anxiety and aggression, during their luteal phase.Q.4. Is there one specific thing I can change in my lifestyle to see the biggest improvement?
Answer: While nutrition is vital, consistent sleep is one of the most powerful tools for cycle relief. There is a statistically significant negative correlation between getting 6 to 8 hours of sleep and the severity of PMS scores. Adequate rest helps stabilize your hormonal rhythms and reduces the stress response that often makes cramps and irritability feel much more intense. If you combine better sleep hygiene with a diet rich in complex carbohydrates and anti-inflammatory nutrients (like those found in bananas, potatoes, and omega-3s), you provide your body with the biological "blueprint" it needs for a smoother cycle.
What References Support This Information?
- Abdullayeva, A., & Shodiyeva, Z. (2025). The impact of hormonal imbalances on female reproductive health: A gynecological perspective. Journal of Modern Educational Achievements, 5, 332–336.
- Ghosh, A., & Muley, A. (2025). Ultra-processed food consumption among college students and their association with body composition, bowel movements and menstrual cycle. International Journal of Public Health, 70, Article 1607712. https://doi.org/10.3389/ijph.2025.1607712
- Lakshmi, N. R., Gopi, K., Kavitha, J., & Kiranmai, P. (2025). Diet and the cycle: Exploring the link between nutrition and premenstrual syndrome. International Journal of Medicine and Public Health, 15(4), 1096–1102. https://doi.org/10.70034/ijmedph.2025.4.196
- Malik, R., Anwar, I., & Ikram, M. (2025). Association between meal skipping and premenstrual syndrome among young females: Meal skipping and premenstrual syndrome. Pakistan Journal of Health Sciences, 6(4), 271–277. https://doi.org/10.54393/pjhs.v6i4.2555
- Parajuli, J., & Prangthip, P. (2025). Adolescent nutrition and health: A critical period for nutritional intervention to prevent long term health consequences. Current Nutrition Reports, 14, Article 116. https://doi.org/10.1007/s13668-025-00706-4
Final Takeaway
Managing PMS and period pain involves a holistic approach that includes understanding your menstrual cycle, addressing dietary habits, and making lifestyle changes. By focusing on reducing sugar and refined carbs, incorporating whole foods and omega-3s, and ensuring meal consistency, you can alleviate symptoms. Additionally, understanding the role of hormones through testing and adopting healthy lifestyle habits like proper sleep and stress management can significantly improve menstrual health. Remember, while PMS symptoms are common, they are not a normal part of life, and addressing them can lead to a healthier and more balanced life.
Book Your Free Consultation
Share this article
Nihala Ibrahim
Nihala Ibrahim is a clinical dietitian with a scientific approach to personalized nutrition and metabolic health. She passionately bridges clinical insights with evidence-based diet strategies to help clients overcome diabetes, thyroid issues, PCOS, and weight challenges for optimal wellness. She holds Masters in clinical dietetics and nutrition science from Sri Ramachandra Institute, Chennai.