How Preconception Nutrition Boosts Fertility for Indian Women
Why Does Preconception Nutrition Matter for Fertility?
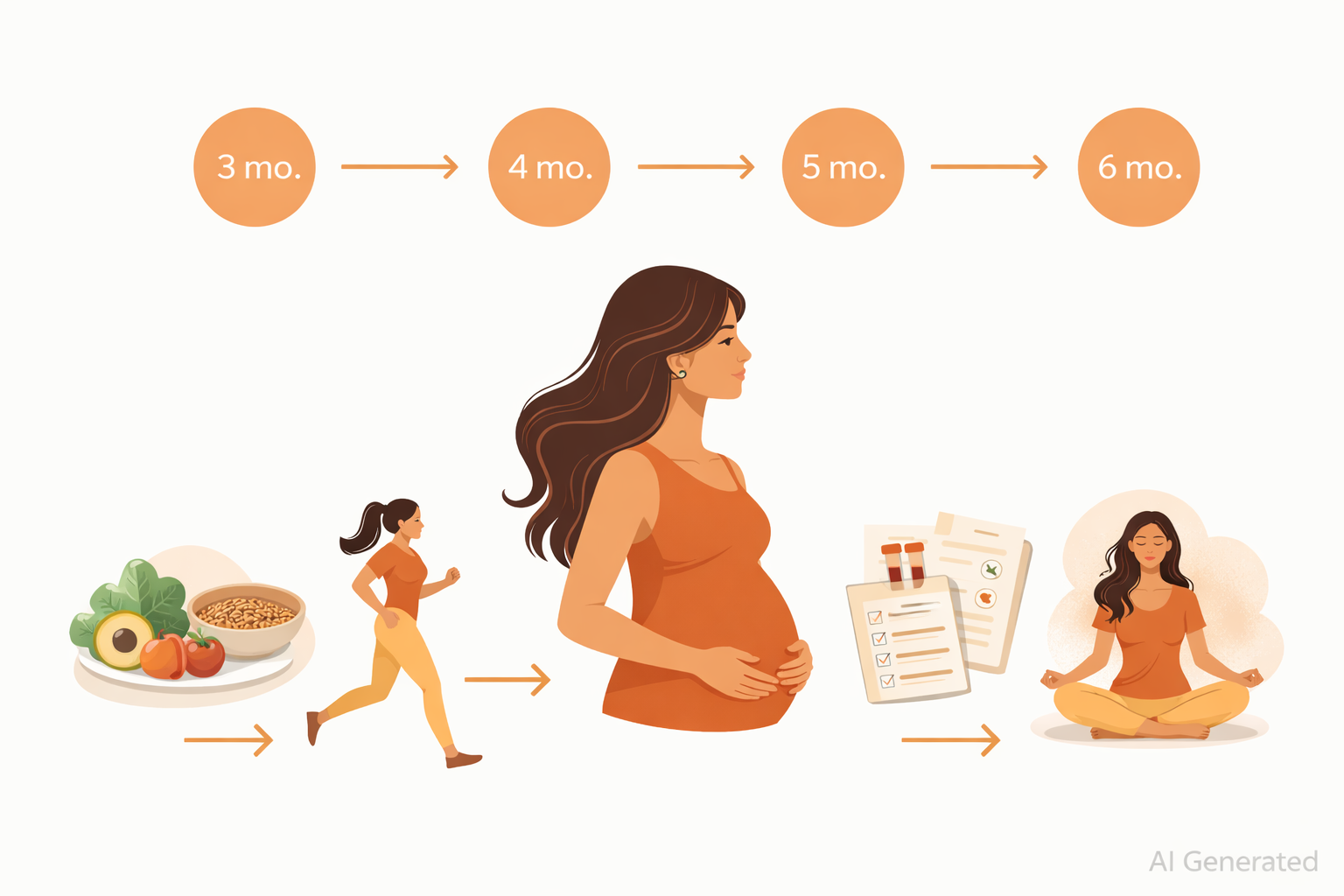
In clinical practice, one of the most common fertility misconceptions is that preparation begins only after conception. Fertility health starts much earlier. Ideally, the body should be prepared at least 3–6 months before trying to conceive. This period is crucial because egg maturation, hormonal balance, and nutritional reserves develop over several months before ovulation occurs.
Preconception nutrition is not just about increasing chances of pregnancy. It plays a critical role in improving egg quality, supporting hormonal regulation, reducing pregnancy complications, and influencing long-term health outcomes for the baby. As discussed in our detailed guide on women’s health core factors , fertility is deeply interconnected with metabolic health, micronutrient status, thyroid function, inflammation, and hormonal balance.
For Indian women, factors such as vegetarian dietary patterns, micronutrient deficiencies, insulin resistance, thyroid disorders, and lifestyle stress make structured fertility preparation even more important. A combination of nutrition planning, blood test evaluation, and genetic insights allows a more personalised and effective fertility approach.
Fertility is deeply influenced by overall metabolic and hormonal health. The nutritional environment within the body directly affects reproductive function.
Ovulation is a hormonally regulated process that depends heavily on nutrient availability. Deficiencies in key vitamins, minerals, and essential fats can impair follicle development and egg maturation. Poor egg quality is a major but often overlooked contributor to fertility challenges and early pregnancy loss.
Balanced nutrition helps regulate:
- Estrogen and progesterone balance
- Insulin sensitivity
- Thyroid hormone function
- Inflammation levels
All these factors influence ovulation consistency and reproductive health.
Preconception nutrition also reduces the likelihood of pregnancy complications such as:
- Gestational diabetes
- Pregnancy-induced hypertension
- Preterm delivery
- Low birth weight
Women who enter pregnancy with balanced nutrient levels and metabolic health are more likely to experience smoother pregnancies and healthier fetal development.
Which Key Nutrients Are Essential for Fertility?
Certain nutrients play a direct role in reproductive function, egg health, and hormone regulation.
- Folate (Folic Acid): Folate is essential for DNA synthesis and cell division. Adequate folate levels reduce neural tube defect risks and support healthy fetal development.
- Iron: Iron supports oxygen transport and energy production. Iron deficiency anemia is highly prevalent among Indian women and is linked to ovulatory dysfunction and fatigue.
- Vitamin B12: Vitamin B12 supports nerve health, red blood cell formation, and DNA synthesis. Vegetarian dietary patterns increase B12 deficiency risk.
- Vitamin D: Vitamin D plays an important role in hormone regulation, ovarian function, and immune balance. Low levels are associated with PCOS, infertility, and poor pregnancy outcomes.
- Omega-3 Fatty Acids: Omega-3 fats reduce inflammation, improve egg quality, and support embryo implantation.
- Iodine: Iodine supports thyroid hormone production, which is critical for ovulation and fetal brain development.
- Zinc and Antioxidants: Zinc supports reproductive hormone production, while antioxidants protect egg cells from oxidative stress.
| Nutrient | Role in Fertility | Food Sources |
|---|---|---|
| Folate (Vitamin B9) | Essential for DNA synthesis, prevents neural tube defects, supports healthy egg development and ovulation | Spinach, fenugreek leaves, lentils, chickpeas, oranges, fortified grains |
| Iron | Prevents anemia, supports oxygen transport to reproductive organs, reduces ovulatory infertility risk | Spinach, beetroot, pomegranate, red meat, eggs, ragi, jaggery |
| Omega-3 Fatty Acids | Reduce inflammation, improve egg quality, regulate reproductive hormones, support uterine blood flow | Flaxseeds, chia seeds, walnuts, fatty fish (salmon, mackerel), fish oil supplements |
| Vitamin D | Regulates menstrual cycles, supports hormone production, improves egg quality and implantation rates | Sunlight exposure (15-20 min daily), fortified milk, egg yolks, mushrooms, supplements |
| Zinc | Critical for cell division, egg maturation, hormone regulation; supports both male and female fertility | Pumpkin seeds, chickpeas, cashews, eggs, dairy, whole grains |
| Vitamin E | Powerful antioxidant that protects eggs from oxidative damage, improves cervical mucus quality | Almonds, sunflower seeds, spinach, avocado, wheat germ oil |
| Vitamin B12 | Supports egg development, prevents miscarriage, works with folate for DNA synthesis | Eggs, dairy products, fortified cereals, meat, fish, nutritional yeast |
| Selenium | Antioxidant that protects eggs and sperm from damage, supports thyroid function (crucial for fertility) | Brazil nuts, eggs, sunflower seeds, whole grains, fish |
| Coenzyme Q10 (CoQ10) | Improves egg quality especially in women over 35, enhances mitochondrial function in eggs | Organ meats, fatty fish, spinach, broccoli, or supplements (200-600 mg daily) |
| Magnesium | Regulates stress hormones, supports progesterone production, reduces inflammation | Pumpkin seeds, almonds, spinach, dark chocolate, bananas, whole grains |
What Are the Recommended Preconception Blood Tests?
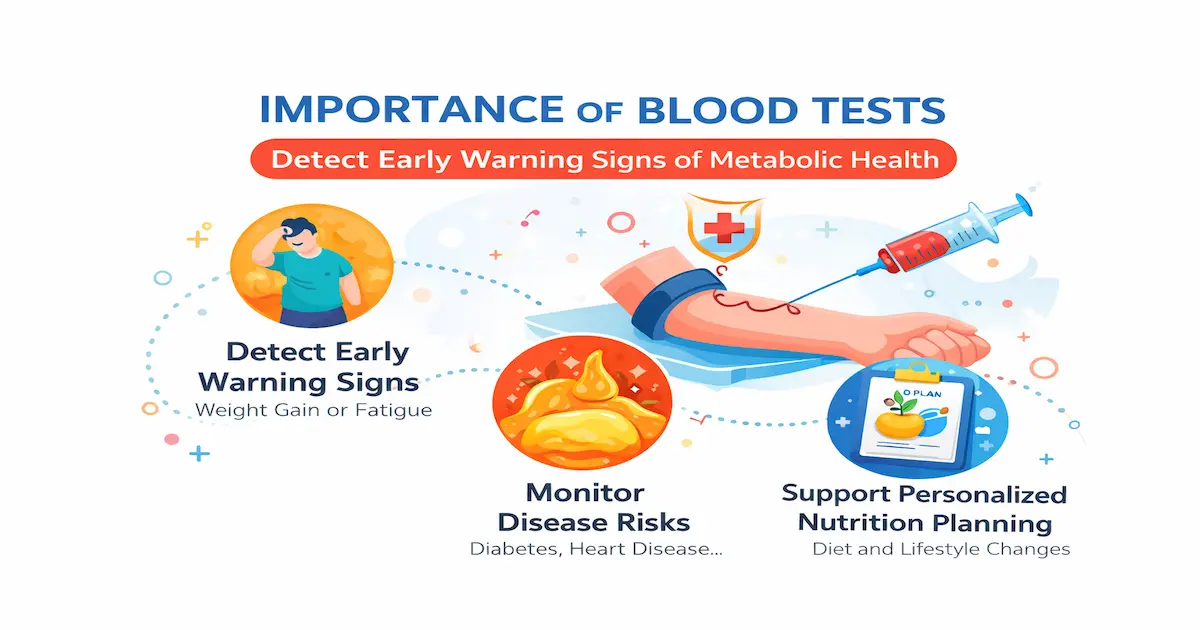
Before planning a pregnancy, understanding the body’s internal health status is extremely important. Many nutritional deficiencies, hormonal imbalances, and metabolic issues remain silent and may not show obvious symptoms. Blood tests act as a powerful screening tool that helps identify hidden deficiencies, hormonal irregularities, inflammation, and metabolic risks that can affect fertility and pregnancy outcomes.
From a fertility perspective, optimal levels of nutrients such as iron, vitamin B12, folate, vitamin D, and thyroid hormones play a major role in supporting ovulation, egg development, implantation, and overall reproductive health. Identifying and correcting imbalances before conception not only improves the chances of pregnancy but also supports healthier fetal development and reduces the risk of complications during pregnancy.
Core Fertility Screening Tests
Certain blood tests are recommended for most women planning pregnancy as they provide a basic overview of nutritional status, metabolic health, and hormonal balance. These tests help detect common deficiencies and disorders that are highly prevalent among Indian women and are known to affect fertility, menstrual regularity, and pregnancy outcomes.

Regular screening allows timely correction through nutrition, supplementation, and lifestyle modifications, helping create a stronger foundation for conception and maternal health.
- Complete Blood Count (CBC) – Detects anemia and overall blood health
- Iron Profile and Ferritin – Evaluates iron stores and deficiency risk
- Vitamin B12 Levels – Supports neurological and reproductive health
- Vitamin D Levels – Essential for hormone balance and immunity
- Thyroid Profile (TSH, T3, T4) – Assesses thyroid function
- HbA1c and Fasting Glucose – Evaluates blood sugar control
- Fasting Insulin – Detects early insulin resistance
Which Additional Tests Are Needed for PCOS or Irregular Cycles?
When women experience irregular menstrual cycles, symptoms of PCOS, unexplained weight gain, insulin resistance, or recurrent fertility challenges, additional diagnostic testing becomes necessary. These specialized tests help evaluate deeper hormonal and metabolic factors that may interfere with ovulation, egg quality, and reproductive hormone balance.
A targeted blood evaluation in such cases allows for more personalized fertility planning. It helps healthcare professionals design nutrition, supplementation, and lifestyle strategies that address the root cause rather than just managing symptoms.
- LH and FSH ratio
- Testosterone levels
- Prolactin
- AMH (Anti-Müllerian Hormone) for ovarian reserve
These tests allow early identification of metabolic or hormonal disturbances that may impact fertility outcomes.
For more information on , please also read: metabolic health blood test
How Does DNA and Nutrigenomics Influence Fertility Planning?
DNA-based fertility planning allows clinicians to move beyond general supplementation and adopt a truly personalised approach. While two women may present with similar fertility challenges, their genetic response to nutrients, hormones, and metabolism may differ significantly.
One of the most researched genetic variations relates to folate metabolism, especially the MTHFR gene. Women with certain variants may struggle to efficiently convert synthetic folic acid into its active form (methylfolate), which is essential for DNA synthesis, embryo development, and neural tube formation. In such cases, simply increasing folic acid intake may not be sufficient, and selecting the bioavailable form becomes crucial.
Genetic markers also influence insulin sensitivity and glucose metabolism, both of which play a major role in ovulation and hormonal balance. Women with genetic predisposition to insulin resistance may experience disrupted ovulation, higher androgen levels, and increased risk of PCOS-related infertility. Identifying this risk early allows for targeted dietary carbohydrate distribution, protein optimisation, and micronutrient support.
Another important aspect is oxidative stress regulation. Egg quality is highly sensitive to oxidative damage, and certain genetic variations reduce the body's natural antioxidant defence systems. DNA testing can highlight the need for higher antioxidant intake through foods rich in vitamins C, E, selenium, zinc, and phytonutrients.
Additionally, genes affecting fat metabolism and inflammation pathways influence reproductive hormone signalling and implantation success. Women with higher inflammatory tendencies may benefit from structured omega-3 intake, anti-inflammatory food patterns, and careful fat selection.
By integrating these genetic insights, fertility nutrition becomes more precise, reducing trial-and-error supplementation and improving overall reproductive readiness.
Please also read our previous blog on DNA based diet for weight loss for Indian women
How Can You Build a Fertility-Friendly Indian Diet Plan?
Traditional Indian diets offer immense fertility-supportive potential when structured correctly. However, modern dietary transitions toward refined grains, processed snacks, and irregular meal patterns often create nutritional gaps that affect reproductive health.
Indian vegetarian diets, while rich in plant diversity, may sometimes fall short in bioavailable iron, vitamin B12, omega-3 fatty acids, and complete protein intake. Strategic food combinations can significantly improve nutrient absorption. For example, pairing lentils or leafy greens with lemon juice or amla enhances iron absorption, while including fermented foods like idli, dosa batter, or homemade curd improves gut health and micronutrient assimilation.
Cooking methods also influence fertility nutrition. Excessive deep frying, prolonged reheating, and high-temperature cooking can damage essential fatty acids and reduce antioxidant content. Preferable methods include steaming, sautéing, pressure cooking, and light roasting, which preserve nutrient density.
In many Indian households, carbohydrate intake tends to dominate meals, with limited protein distribution across the day. For fertility optimisation, including protein in every major meal helps stabilise blood sugar, regulate insulin, and support hormone synthesis. Foods such as dals, paneer, tofu, eggs, fish, sprouts, and nuts can be distributed strategically throughout the day.
Hydration and traditional beverages also play a role. Buttermilk, coconut water, herbal infusions, and jeera or fennel water can support digestion and mineral balance while reducing reliance on caffeinated beverages.
| Plate Component | Percentage of Plate | Food Sources (Indian Options) | Fertility Benefit |
|---|---|---|---|
| High-Quality Protein | 25% | Paneer, tofu, eggs, chicken, fish, lentils | Supports hormone production, egg quality, and stable blood sugar |
| Whole Grains / Millets | 25% | Brown rice, quinoa, bajra, jowar | Provides sustained energy, supports insulin balance, and improves nutrient density |
| Vegetables | 40% | Leafy greens, colourful vegetables (carrot, beetroot, capsicum, broccoli, etc.) | Rich in antioxidants, fiber, folate, and micronutrients that support reproductive health |
| Healthy Fats | 10% | Nuts, seeds, ghee, cold-pressed oils | Supports hormone synthesis, reduces inflammation, and improves nutrient absorption |
Table: Ideal Fertility-Supporting Plate Structure for Indian Women
What Does a Sample Day of Eating Look Like for Fertility?
| Meal | Food Items | Nutritional Focus |
|---|---|---|
| Waking Up | Warm water with soaked fenugreek seeds OR herbal tea with ginger | Hydration, detoxification, hormone balance |
| Breakfast | Vegetable moong chilla with paneer filling, Mint chutney, 1 Glass Buttermilk | Protein, complex carbs, B vitamins, probiotics |
| Mid-Morning | Handful of soaked almonds and walnuts + Fruit Bowl + Pumpkin Seeds (10g) | Healthy fats (omega-3), antioxidants, Vitamin E |
| Lunch | 1 cup brown rice/3 Multi grain Rotis, mixed dal/grilled fish/chicken, palak paneer, cucumber raita, mixed vegetable salad | Complete protein, iron, folate, calcium, fiber, probiotics |
| Evening Snacks | Sprouted moong chaat with lemon and spices OR roasted makhana with turmeric or roasted chana/homemade trail mix with herbal tea | Plant protein, antioxidants, anti-inflammatory compounds |
| Dinner | vegetable Khichadi, Curd, vegetable salad or soup | Iron, folate, fiber, complex carbs, antioxidants |
| Before Bed | Warm turmeric milk with a pinch of cinnamon OR ashwagandha moon milk | Anti-inflammatory, stress reduction, sleep quality, hormone regulation |
Which Foods Should You Minimise for Better Fertility?
Following foods/habits can increase inflammation and disrupt hormonal balance.
- Trans fats and fried foods
- Sugary beverages and refined desserts
- Excess caffeine
- Smoking and alcohol
- Ultra-processed packaged foods
Key Food Groups That Support Preconception and Fertility
| Food Group | Nutritional Benefits | Recommended Sources |
|---|---|---|
| Whole Grain | Provide complex carbohydrates for stable blood sugar and energy; rich in B vitamins for hormonal balance | Brown rice, jowar, bajra, ragi, whole wheat, quinoa, oats |
| Protein Rich Foods | Support egg quality, hormone production, and tissue repair; essential amino acids for reproductive health | Moong dal, masoor dal, chickpeas, paneer, Greek yogurt, eggs, chicken, fish |
| Health Fats | Aid hormone synthesis, reduce inflammation, improve egg quality and ovulation | Ghee, coconut oil, nuts (almonds, walnuts), seeds (flax, chia, pumpkin), fatty fish |
| Leafy Greens & Vegetables | High in folate, iron, antioxidants; support uterine health and reduce oxidative stress | Spinach, fenugreek leaves, amaranth, broccoli, bell peppers, carrots, beetroot |
| Fruits | Rich in antioxidants (Vitamin C, E) that protect egg and sperm quality; support immune function | Berries, pomegranate, papaya, oranges, guava, apples, bananas |
| Dairy & Alternatives | Provide calcium, Vitamin D, probiotics for gut health; support bone health and hormone regulation | Curd, buttermilk, paneer, cheese, fortified plant milks (almond, soy) |
| Herbs & Spices | Anti-inflammatory properties, balance hormones, improve circulation to reproductive organs | Turmeric, ginger, cinnamon, fenugreek seeds, shatavari, ashwagandha |
How Do Weight and PCOS Affect Fertility?
Body weight and metabolic health have a direct influence on ovulation, hormone balance, and pregnancy outcomes. Both excess weight and being underweight can disrupt reproductive signaling.
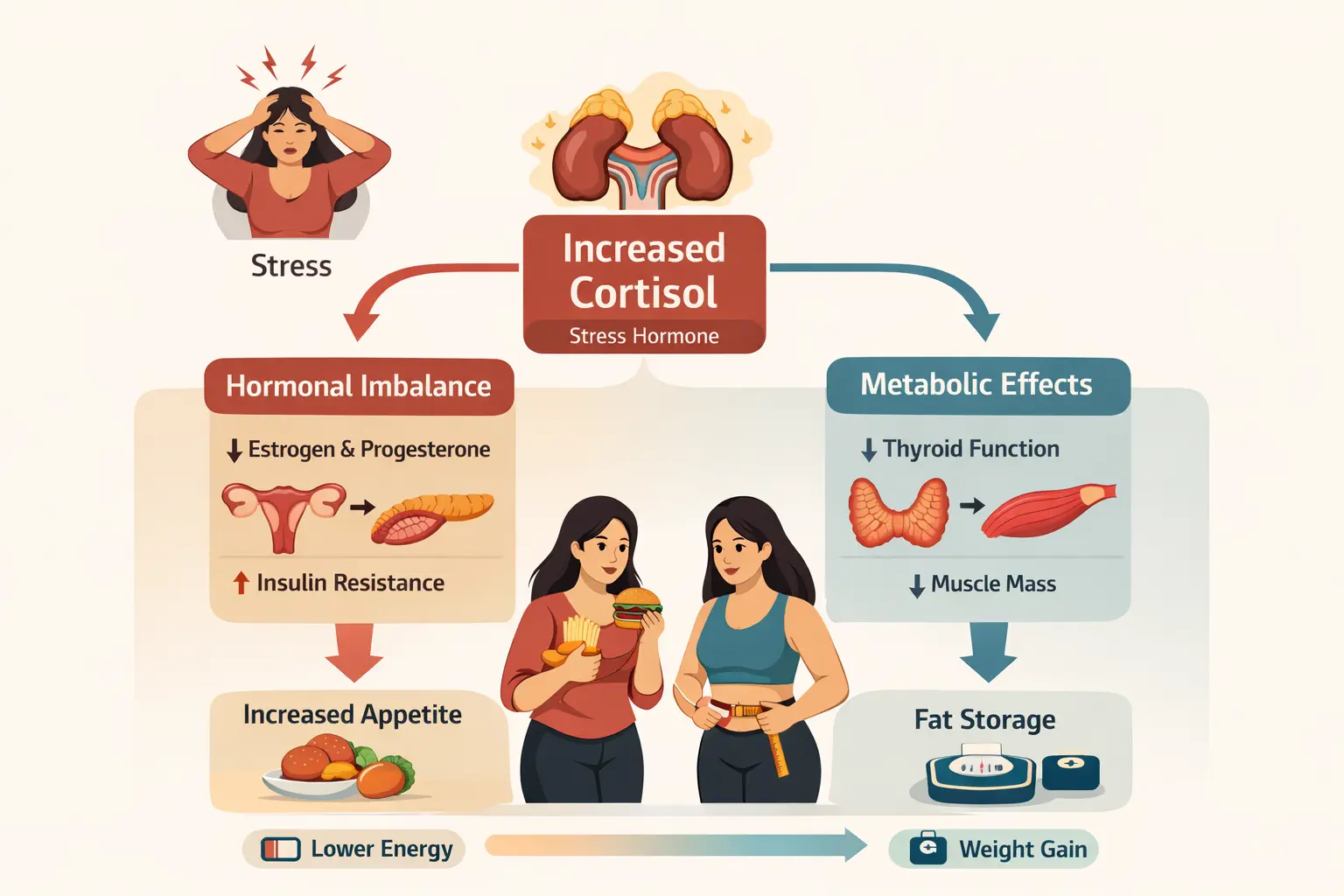
Excess body fat, particularly abdominal fat, contributes to increased production of inflammatory cytokines and insulin resistance. Elevated insulin levels stimulate ovarian androgen production, which interferes with follicle maturation and ovulation. This is one of the primary mechanisms behind infertility in women with PCOS.
Even modest weight reduction of 5–10% of body weight has been shown to improve ovulatory cycles, insulin sensitivity, and pregnancy outcomes in women with PCOS. However, aggressive calorie restriction or crash dieting can worsen hormonal imbalance, increase cortisol levels, and negatively impact egg quality.
A personalized weight management approach focusing on stable blood sugar, adequate protein intake, anti-inflammatory foods, and structured physical activity provides more sustainable reproductive benefits than rapid weight loss.
For women who are underweight, insufficient fat stores can suppress estrogen production and disrupt menstrual cycles. In such cases, improving calorie quality, increasing healthy fat intake, and restoring muscle mass becomes equally important.
What Lifestyle Factors Impact Fertility Success?
Lifestyle plays a critical role in reproductive success and often determines how effectively nutrition supports fertility.
Sleep and Circadian Rhythm
Sleep regulates melatonin production, which acts as a powerful antioxidant protecting egg quality. Chronic sleep deprivation can disrupt insulin sensitivity, increase cortisol, and impair reproductive hormone balance. Maintaining consistent sleep schedules and reducing late-night screen exposure helps support hormonal rhythm.
Stress and Cortisol Regulation
Chronic psychological stress increases cortisol levels, which can interfere with ovulation and progesterone balance. Stress also affects digestive efficiency and nutrient absorption. Incorporating relaxation practices such as breathing exercises, yoga, meditation, or mindful movement can improve hormonal stability and reproductive readiness.
Environmental Toxins and Endocrine Disruptors
Exposure to environmental chemicals such as BPA (found in plastics), pesticides, heavy metals, and certain cosmetic ingredients can mimic or block natural hormones. Long-term exposure has been linked to reduced fertility, PCOS risk, and thyroid dysfunction.
Practical steps include:
- Reducing plastic food storage and switching to glass or steel containers
- Washing fruits and vegetables thoroughly
- Choosing clean personal care and cosmetic products
- Avoiding reheating food in plastic containers
Physical Activity
Moderate exercise improves insulin sensitivity, blood circulation to reproductive organs, and stress regulation. However, excessive high-intensity training without adequate nutrition may suppress ovulation. Balanced routines combining strength training, walking, yoga, and flexibility work provide optimal fertility support.
What Are the Final Thoughts on Preconception Nutrition?
Fertility is influenced by multiple factors, and preparing for pregnancy goes far beyond simply planning the timing of conception. A woman’s nutritional status, hormonal balance, metabolic health, genetic predispositions, and lifestyle habits together create the foundation for reproductive health. Addressing these factors proactively can significantly improve conception outcomes and support a healthier pregnancy journey.
Preconception planning offers an opportunity to correct nutritional deficiencies, stabilise blood sugar levels, optimise thyroid and hormonal function, and build adequate nutrient reserves required for both maternal and fetal health. Even small improvements made during this preparation phase can positively influence egg quality, implantation success, pregnancy complications, and long-term health outcomes for the baby.
For Indian women, where micronutrient deficiencies, vegetarian dietary patterns, metabolic disorders, and lifestyle stress are common, structured fertility preparation becomes even more valuable. Combining detailed blood test evaluation with personalised nutrition strategies and, where needed, nutrigenomic insights allows for a more targeted and effective approach rather than relying on general fertility advice.
Fertility preparation is not about perfection but about creating the healthiest possible environment for conception and pregnancy. Taking time to prepare the body before trying to conceive is an investment in both maternal well-being and the future health of the child.
References
- Preconception Health and Health Care – WHO Guidelines
- Nutrition and Female Fertility: An Interprofessional Approach
- Micronutrients and Female Fertility
- Nutrigenomics and Reproductive Health
Final Takeaway
What Are Common FAQs About Preconception Nutrition and Fertility?
- How early should I start fertility nutrition?
Answer: Ideally, fertility preparation should begin 3–6 months before conception, as egg development occurs over several months.
- Can fertility improve with diet alone?
Answer: Nutrition significantly influences fertility, but results are best when combined with lifestyle modifications and medical evaluation.
- Are supplements necessary before pregnancy?
Answer: Supplement needs depend on blood test results. Common supplements include folate, vitamin D, iron, and B12.
- Can weight loss improve fertility in PCOS?
Answer: Yes. Even 5–10% weight reduction can improve ovulation and hormonal balance.
- Is DNA testing essential for fertility planning?
Answer: DNA testing is not mandatory but helps personalise diet and supplement strategies, especially in cases of repeated fertility challenges.
- Can stress affect fertility?
Answer: Yes. Chronic stress can suppress ovulation and alter hormone balance.
- Should men also follow preconception nutrition?
Answer: Yes. Male nutrition influences sperm quality and overall fertility outcomes.
Final Takeaway
Preconception nutrition is a vital component of fertility planning for Indian women. By addressing nutritional deficiencies, understanding genetic predispositions, and making informed lifestyle choices, women can create a supportive environment for conception and a healthy pregnancy. Personalized approaches that consider individual health status, dietary patterns, and lifestyle factors can significantly enhance fertility outcomes and promote long-term health for both mother and child.
Book Your Free Consultation
Share this article
Nupur Sharma
Nupur Sharma is a Sports Nutritionist. She has a scientific approach towards nutrition. She passionately unfolds latent aspects linking nutritional science and sports performance so that athletes and fitness enthusiasts can achieve their highest potential. She holds a Master’s degree in Sports Nutrition and Bachelor’s degree in Food, Nutrition and Dietetics.