Vitamin D Deficiency: Symptoms, Causes and Diet
Vitamin D Deficiency: Symptoms, Causes and Diet
Vitamin D has gained significant attention in recent decades as research continues to uncover its vital role in human health. Often called the "sunshine vitamin," it is actually a pro-hormone that your body produces when skin is exposed to sunlight. Despite its importance, vitamin D deficiency is a high-prevalence public health problem worldwide.
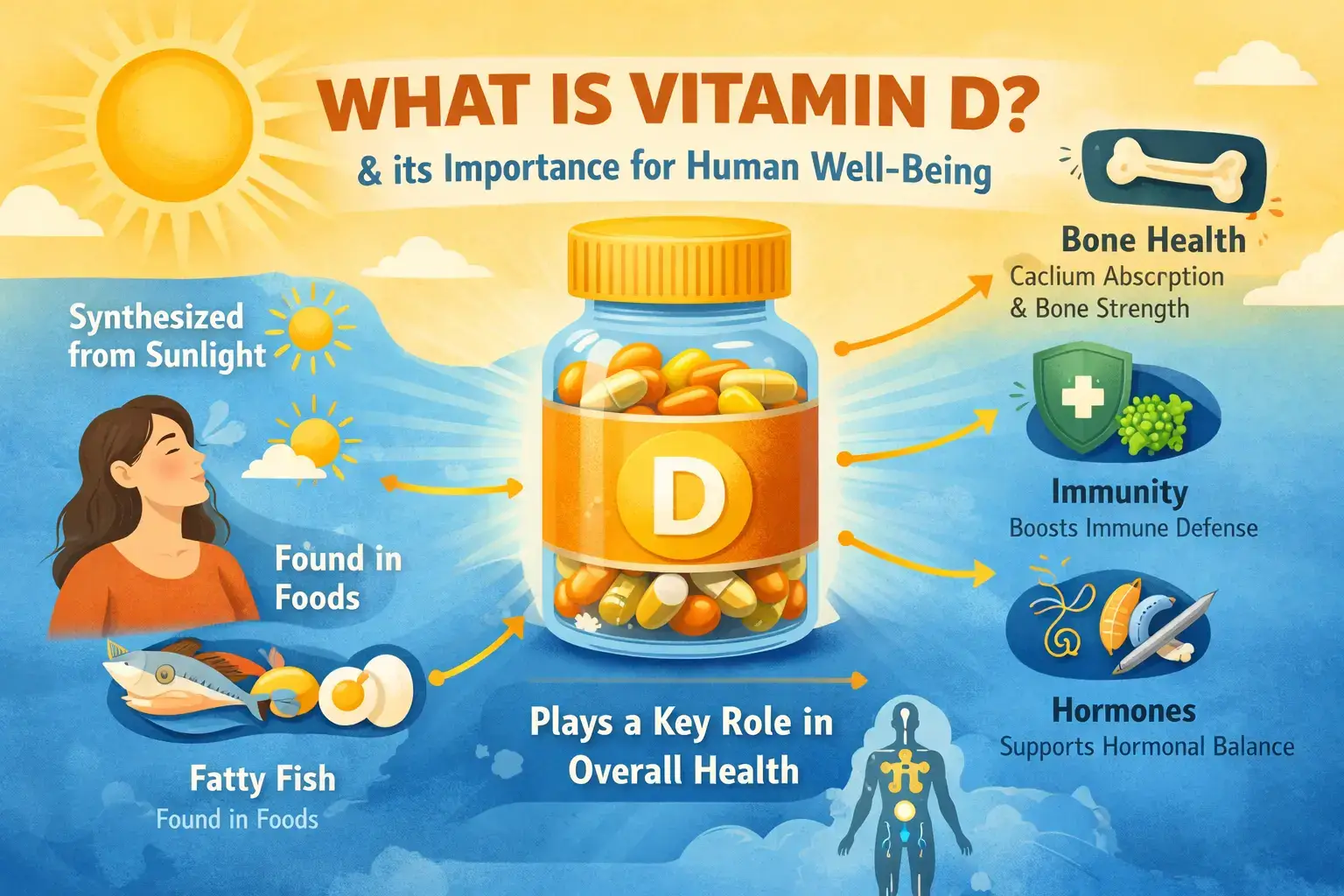
What is Vitamin D?
Vitamin D is a nutrient crucial for musculoskeletal health, playing a central role in regulating bone and mineral metabolism. It exists in two main forms: Vitamin D3 (cholecalciferol), which is synthesized in the skin or found in animal products, and Vitamin D2 (ergocalciferol), which is typically plant-derived.
Once it enters the body, vitamin D is converted by the liver into 25-hydroxyvitamin D (25(OH)D), which is the metabolite measured in blood tests to determine your status. From there, the kidneys and other tissues transform it into 1,25-dihydroxyvitamin D, a powerful steroid hormone that exerts effects on almost every cell in the human body.
The Causes of Deficiency: Lifestyle and Genetics
While our bodies are designed to produce vitamin D naturally, several factors can interfere with this process.
- Lifestyle Factors: Modern lifestyles often involve significant time spent indoors, leading to low sun exposure. Factors such as living at high latitudes, where UV-B rays are weaker, or using excessive sun protection can further reduce the skin's ability to synthesize the vitamin. Additionally, dietary intake is usually a minor source, providing only about 100 to 200 IU per day for the average person.
- Genetics: Not everyone processes vitamin D the same way. Genetic polymorphisms can influence an individual’s sensitivity to vitamin D and how their body responds to supplementation. In rare cases, genetic disorders like inherited 24-hydroxylase deficiency can cause an inability to properly break down vitamin D metabolites, leading to toxicity even at normal doses.
- Biological and Health Factors: Obesity is a major factor, as vitamin D is fat-soluble and can be "sequestered" in adipose tissue, making it less available in the bloodstream. People with darker skin pigmentation also have a harder time synthesizing vitamin D from sunlight. Conditions that cause malabsorption, such as celiac disease, inflammatory bowel disease (IBD), or bariatric surgery, also significantly increase the risk of deficiency.
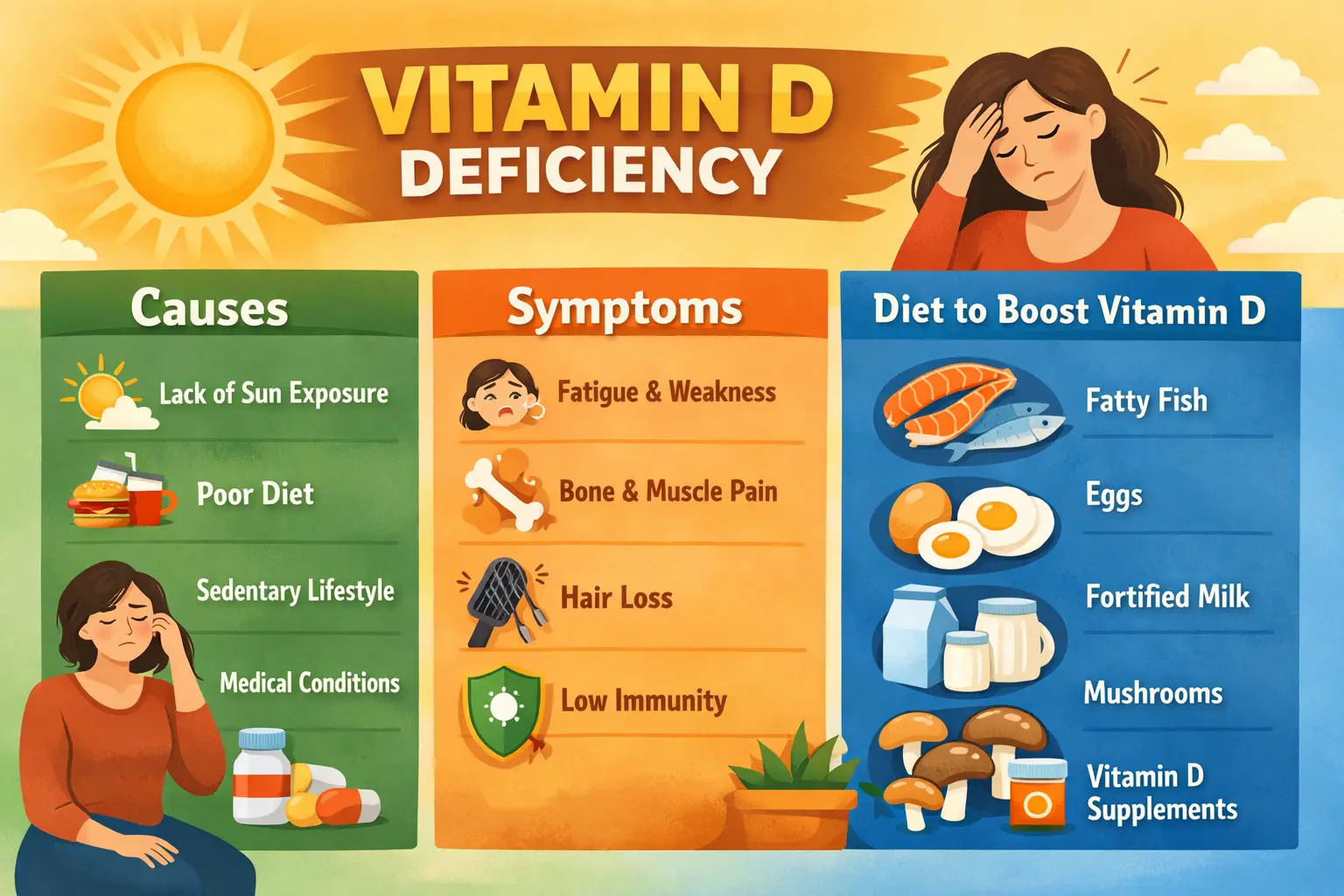
Symptoms: The Quiet Warning Signs
Vitamin D deficiency can be subtle, often showing no obvious symptoms until it becomes severe.
- Bone and Muscle Issues: Chronic deficiency can lead to rickets in children and osteomalacia (softening of the bones) in adults.
- Pain and Mobility: Many people experience musculoskeletal pain or general muscle weakness.
- Increased Risks: Low levels are strongly associated with an increased risk of falls and fractures, especially in older adults.
- Extra-Skeletal Links: Observational studies have linked low vitamin D to a variety of other conditions, including metabolic syndrome, cardiovascular disease, autoimmune disorders, and respiratory infections.
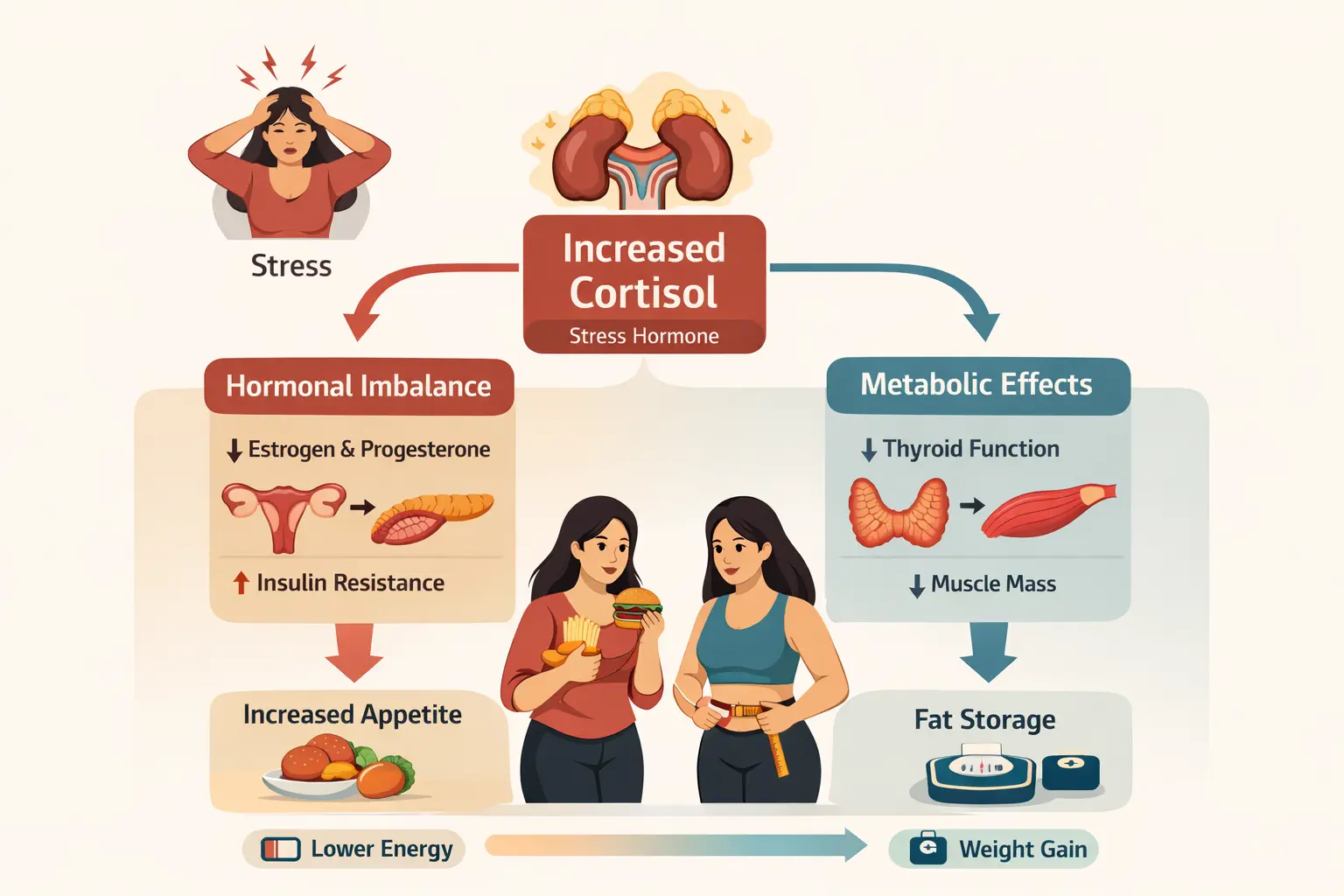
Vitamin D deficiency is also closely linked to insulin resistance, a key driver of metabolic disorders such as type 2 diabetes and PCOS. Vitamin D plays an important role in insulin sensitivity by supporting insulin receptor function and reducing low-grade inflammation. When vitamin D levels are low, the body’s ability to use insulin efficiently may decline, leading to higher blood sugar levels and increased fat storage over time. This is one reason why individuals with persistent vitamin D deficiency often struggle with weight management and metabolic health. Understanding this connection helps explain why correcting vitamin D levels can be an important part of improving insulin sensitivity and overall metabolic balance.
It’s important to note that persistent fatigue in women is often not caused by vitamin D deficiency alone. Iron deficiency and low haemoglobin levels commonly coexist and can significantly worsen exhaustion. Read more about iron deficiency and chronic fatigue in women .
Hormonal and Metabolic Testing
Because vitamin D acts as a hormone and affects mineral balance, doctors use specific blood and DNA tests to assess your health.
- 25(OH)D Blood Test: This is the standard laboratory marker used to diagnose deficiency.
- Deficiency: Below 20 ng/mL (50 nmol/L).
- Insufficiency: 20 to 30 ng/mL (50–75 nmol/L).
- Sufficiency: 30 to 50 ng/mL (75–125 nmol/L).
- Metabolic Panel: In cases of severe deficiency, clinicians may also test for serum calcium, phosphate, alkaline phosphatase, parathyroid hormone (PTH), creatinine, and magnesium to get a full picture of your hormonal and mineral balance.
- DNA/Genetic Testing: For patients who show unusual responses to treatment or signs of toxicity, genetic analysis may be used to confirm rare inherited disorders.
Treatment and Nutrition Tips
Achieving a healthy vitamin D status requires a combination of lifestyle changes and, often, supplementation.
Nutrition and Lifestyle Tips:
- Consume Vitamin D-Rich Foods: Focus on natural or fortified sources, such as fatty fish and fortified dairy products.
- Support Bone Health with Calcium: Ensure adequate dietary calcium intake through milk, yogurt, and cheese, as calcium and vitamin D work together to protect your bones.
- Safe Sun Exposure: Moderate and cautious sunlight exposure is an effective way to improve vitamin D status naturally.
- Manage Weight: Because obesity can lower available vitamin D, maintaining a healthy weight through physical activity is recommended.
FAQs: Common Questions Answered
- Can I get enough Vitamin D just from my diet?
It is very difficult. Most people get only 100–200 IU daily from food, whereas many experts recommend 800–2000 IU to maintain healthy levels. Supplementation or sunlight exposure is usually necessary.
- Is Vitamin D3 better than Vitamin D2?
Yes, research generally prefers Vitamin D3 (cholecalciferol) over Vitamin D2 (ergocalciferol) because it is more effective at raising and maintaining serum vitamin D levels.
- Can you take too much Vitamin D?
Yes, vitamin D oversupply can lead to toxicity, which may cause high calcium levels (hypercalcemia), kidney issues, and vascular calcification. However, toxicity is rare and typically only occurs when blood levels exceed 150 ng/mL
- How long does it take to correct vitamin D deficiency?
The time needed to improve vitamin D levels depends on how low your levels are, your sun exposure, diet, body weight, and whether you are taking supplements. In many cases, noticeable improvement in blood levels can take 8–12 weeks with consistent supplementation and lifestyle changes, though some individuals may require longer-term management.
- Should vitamin D levels be tested regularly?
Yes. Periodic testing is recommended, especially for individuals at higher risk of deficiency such as those with limited sun exposure, obesity, malabsorption conditions, or hormonal and metabolic disorders. Regular testing helps ensure levels remain within a healthy range and avoids both deficiency and excess.
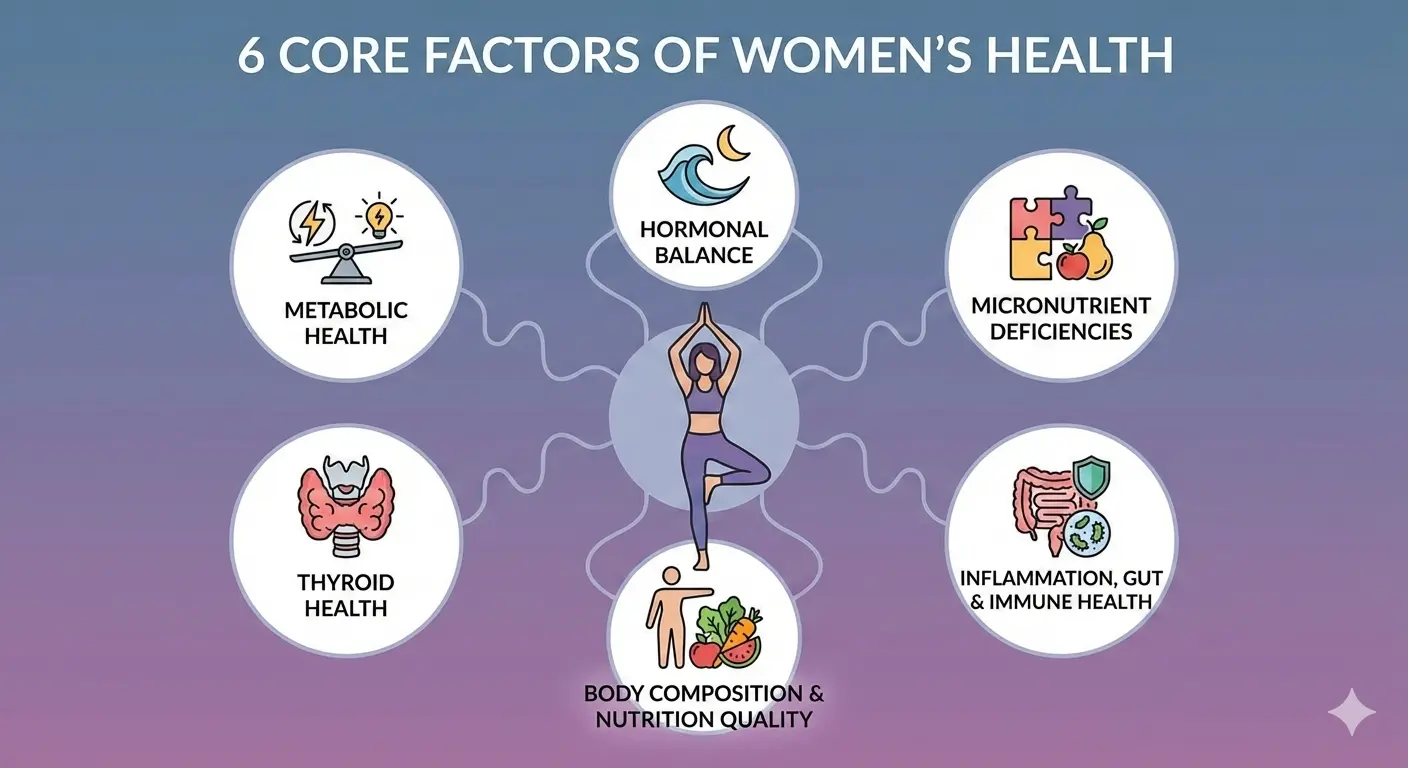
This topic is one important aspect of women’s health, but it does not exist in isolation. Metabolic health, hormonal balance, nutrient status, thyroid function, body composition, gut health and inflammation are deeply interconnected.
To understand how this fits into the bigger picture, read our comprehensive guide on Women’s Health Explained: 6 Core Factors That Influence Hormones, Metabolism & Long-Term Health , which outlines a holistic framework for long-term women’s wellbeing.
Vitamin D deficiency rarely exists in isolation. It often overlaps with hormonal imbalance, insulin resistance, thyroid dysfunction, and chronic inflammation—especially in women. Understanding vitamin D status as part of a broader health framework is essential for long-term results.
In our pillar guide, Women’s Health Explained: 6 Core Factors That Influence Hormones, Metabolism & Long-Term Health , we explain how micronutrient deficiencies like vitamin D interact with metabolic health, hormonal balance, thyroid function, and inflammation rather than acting alone.
Final Takeaway
Encourage readers to book a FREE consultation with unlock.fit to understand DNA-based personalised nutrition. Tone must be educational, not salesy.
Vitamin D needs can vary significantly based on genetics, lifestyle, and metabolic health. If you’re dealing with persistent deficiency or unsure whether your current approach is working, a personalised plan can help. At unlock.fit, you can book a free consultation to understand how your DNA, nutrition, and lifestyle influence your vitamin D levels—so you can make informed, targeted choices for long-term health.
References
Pludowski, P., Takacs, I., Boyanov, M., Belaya, Z., Diaconu, C. C., Mokhort, T., Zherdova, N., Rasa, I., Payer, J., & Pilz, S. (2022).
Clinical Practice in the Prevention, Diagnosis and Treatment of Vitamin D Deficiency: A Central and Eastern European Expert Consensus Statement.
Nutrients, 14(7), 1483.
https://doi.org/10.3390/nu14071483
Zemp, J., Erol, C., Kaiser, E., Aubert, C. E., Rodondi, N., & Moutzouri, E. (2025). A systematic review of evidence-based clinical guidelines for vitamin D screening and supplementation over the last decade. Archives of Public Health, 83, 221. https://doi.org/10.1186/s13690-025-01709-x
Book Your Free Consultation
Share this article
Nihala Ibrahim
Nihala Ibrahim is a clinical dietitian with a scientific approach to personalized nutrition and metabolic health. She passionately bridges clinical insights with evidence-based diet strategies to help clients overcome diabetes, thyroid issues, PCOS, and weight challenges for optimal wellness. She holds Masters in clinical dietetics and nutrition science from Sri Ramachandra Institute, Chennai.