What Is Insulin Resistance? Symptoms, Causes & Diet
What Is Insulin Resistance? Symptoms, Causes & Diet
If you have ever felt constantly tired after a meal, struggled with weight that seems impossible to shift, or been told your “blood sugar is a bit high,” you might be dealing with insulin resistance (IR). Often called a silent metabolic condition, insulin resistance affects how your body uses energy and plays key role in conditions like type 2 diabetes, fatty liver, PCOS, and heart disease.
What is Insulin Resistance?
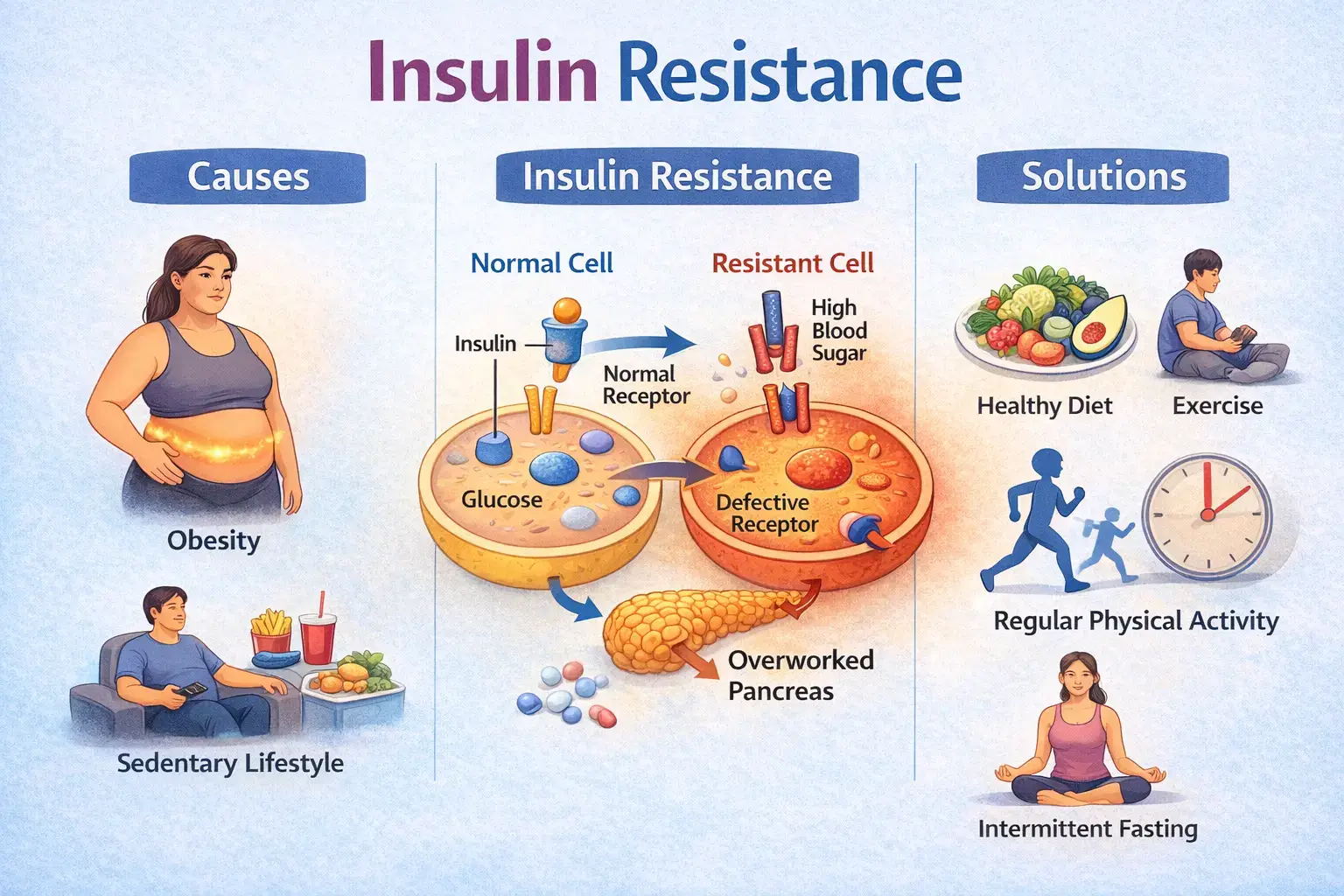
At its simplest level, insulin is a hormone that acts like a key. Its job is to unlock your body’s cells (primarily in your liver, muscles, and fat tissue) so they can take in glucose (sugar) from your blood to use for energy.
When you have insulin resistance, your cells begin to “ignore” or resist the signal from this hormone. Imagine the lock on the cell door is jammed; the insulin key still exists and the cells aren’t taking in the sugar, your blood sugar levels stay high. To compensate, your pancreas works overtime to pump out even more insulin (this state is called hyperinsulinemia) to force those “locks” to open and keep your blood sugar stable.
Eventually the pancreas can’t keep up, leading to pre-diabetes or overt Type 2 Diabetes (T2DM). Beyond blood sugar, IR is a “hotbed” that breeds other issues, including obesity, non-alcoholic fatty liver disease (NAFLD), heart disease, and polycystic ovary syndrome (PCOS).
Why Does the “Key” Stop Working?
It is typically a blend of genetics, environment, and lifestyle. Key drivers include:
Obesity & Abdominal Fat:
The primary factor. Visceral fat acts as an active organ, releasing inflammatory chemicals and free fatty acids that “clog” cell receptors and disrupt insulin signaling.
Sedentary Lifestyle:
Inactivity directly lowers muscle sensitivity to insulin.
Genetics: 3 Genetic Drivers of Insulin Resistance
- Insulin Receptor Mutations (INSR Gene): Genetic flaws can cause “broken locks” on your cells. Even with plenty of insulin, the receptors are either too few or too misshapen to bind with the hormone, preventing glucose entry.
- Post-Receptor Signaling Defects (IRS-1/2 Genes): In this case, the “lock” works, but the “internal wiring” is faulty. Variations in these genes disrupt the chemical signal after insulin docks, meaning the message to let sugar in never reaches the rest of the cell.
- Fat Distribution Genetics (PPARG Gene): Your genes dictate where you store fat. Variants in the PPARG gene can cause the body to store fat in “dangerous” places like the liver and muscles (ectopic fat) rather than under the skin, triggering localized insulin resistance.
Aging:
Natural declines in mitochondrial function and increased fat storage in the liver and muscles contribute to IR over time.
Dietary Habits:
IR is linked to energy-dense foods, skipping breakfast, irregular meal timing, and late-night eating.
Nutrient Deficiencies:
A lack of Vitamin D, Magnesium, or Calcium can accelerate Insulin Resistance. Vitamin D is particularly vital for regulating insulin secretion and sensitivity.
Medications:
Certain drugs, such as steroids (glucocorticoids) or anti-rejection meds, can trigger IR as a side effect.
Symptoms of Insulin Resistance
Insulin resistance is often called “silent” because it doesn’t always have obvious outward symptoms in the early stages. However, your body often leaves clues:
- Increased Waist Circumference.
- Hypertriglyceridemia: High levels of triglycerides and low levels of “good” (HDL) cholesterol.
- Acanthosis Nigricans: IR is associated with systemic inflammation and hormone imbalances that can affect skin and energy levels.
- Fatigue and Brain Fog.
- High Blood Pressure.
Dietary Changes: The Roadmap to Reversal
The good news is that IR is often manageable through lifestyle interventions, with diet being the “cornerstone” of treatment.
- Prioritize Weight Loss (Even a Little)
A weight loss of just 7% to 10% of your initial body weight can significantly improve insulin sensitivity and potentially lead to the remission of Type 2 Diabetes. The best approach is an individualized plan that creates a consistent energy deficit.
- Manage Your Carbohydrates
It’s not just about “no carbs,” but rather the quality and quantity.
Low GI and GL: Choose foods with a low Glycemic Index (GI) and Glycemic Load (GL), such as whole grains, legumes (beans/lentils), and pasta. These cause a slower, smaller rise in blood sugar.
Fiber is Key: Increasing fiber by 15-35 grams a day reduces IR markers and inflammation. Whole grain cereal products, fruits, and vegetables are excellent sources.
- Follow a “Meal Sequence”
The order in which you eat your food matters. Research shows that eating low-density foods first can “buffer” the insulin response.
Start with: Vegetables, salads, or soups.
Follow with: Proteins (fish, poultry, eggs, or plant proteins like tofu) and healthy fats (olive oil, nuts).
Finish with: Starchy foods or carbohydrates. This sequence delays gastric emptying, meaning the sugar from your meal hits your bloodstream much more slowly.
- Master Chrononutrition (Meal Timing)
Your body follows a 24-hour clock, and your insulin sensitivity is naturally higher in the morning and lower at night.
Consuming at least half of your daily carbohydrates at lunch time and avoiding heavy meals in the late evening can improve your 24-hour glucose peaks.
- Consider Intermittent Fasting or TRF
Time-Restricted Feeding (TRF) involves eating your meals within a specific window (e.g., a 10-hour window like 8:00 AM to 6:00 PM). This creates a longer daily fasting period, which allows your insulin levels to drop low enough for your body to start burning stored fat and ketone bodies for energy.
Certain common ingredients have been shown to offer extra help:
- Vinegar: Consuming vinegar (like apple cider vinegar) as a dressing or diluted in a drink before a carb-rich meal can slow digestion and reduce blood sugar spikes.
- Yogurt and Fermented Foods: These may improve insulin sensitivity through their beneficial bacteria and organic acids.
- Whey Protein or high-quality protein sources: Having a small amount of whey protein before a meal can stimulate the hormones that tell your body to release insulin more efficiently.
- Nuts: Peanuts and tree nuts (like pistachios and walnuts) are rich in antioxidants and healthy fats that support insulin signalling.
While diet is vital, exercise is the other half of the equation.
- The Power of Both: Combining aerobic exercise (brisk walking, swimming) with resistance training (weightlifting) is more effective than either alone.
- Muscle is a Glucose Sponge: Strength training increases your muscle mass; since muscles are responsible for 80% of your body’s glucose uptake, having more (and higher quality) muscle mass gives that sugar a place to go.
- Post-Meal Walks: Even a brief 10-minute walk after eating can help lower postprandial (post-meal) blood sugar.
Frequently Asked Questions:
Q1. Can insulin resistance actually be reversed, or will I eventually get diabetes?
Insulin resistance is often reversible or manageable, and its progression to Type 2 Diabetes (T2DM) is not inevitable. Lifestyle interventions are the “cornerstone” of treatment, and achieving a weight loss of just 7% to 10% of your initial body weight can significantly improve insulin sensitivity and even lead to the remission of T2DM
Q2. Does it really matter “when” I eat if I am eating the right foods?
Yes, timing is critical because your body follows a 24-hour internal clock known as chrononutrition. Insulin sensitivity naturally peaks in the morning and mid-day (around 10:00 AM) and is significantly lower in the evening and night. Eating a heavy meal late at night triggers metabolic stress and “circadian misalignment,” which makes your cells more resistant to insulin the following morning.
Q3. Why is my “waist size” such a big deal for insulin resistance?
Your waist circumference is a reliable marker of the severity of insulin resistance because it measures visceral fat. Unlike fat stored under the skin, visceral fat around the abdominal organs is biologically active; it pumps out inflammatory chemicals and “free fatty acids” that directly interfere with the insulin signaling pathway
Q4. Are there any “superfoods” or vitamins that can help fix the problem?
While there is no magic pill, certain functional foods and nutrients can offer significant support:
- Vinegar: Consuming vinegar (like apple cider vinegar) before or with a carb-rich meal can delay gastric emptying and reduce blood sugar spikes.
- Fiber: Increasing daily fiber by 15–35 grams can reduce inflammation and improve insulin sensitivity.
- Protein source: Stimulate the body to release insulin more efficiently.
- Vitamin D: Deficiency in Vitamin D is a known factor that accelerates the development of insulin resistance.
Q5. What is the difference between Insulin Resistance and Type 2 Diabetes Miletus.
Insulin resistance is a physiological state where cells ignore insulin, often compensated for by higher insulin production.1 Type 2 Diabetes (T2DM) is a clinical diagnosis occurring when the pancreas can no longer overcome this resistance, causing blood sugar to reach diagnostic thresholds (HbA1c > 6.5%)
Sources:
- https://doi.org/10.3390/nu14040823
- https://doi.org/10.3389/fendo.2023.1149239
- https://doi.org/10.3390/nu13103491
Book Your Free Consultation
Share this article
Nihala Ibrahim
Nihala Ibrahim is a clinical dietitian with a scientific approach to personalized nutrition and metabolic health. She passionately bridges clinical insights with evidence-based diet strategies to help clients overcome diabetes, thyroid issues, PCOS, and weight challenges for optimal wellness. She holds Masters in clinical dietetics and nutrition science from Sri Ramachandra Institute, Chennai.